Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: To present eight patients with progressive supranuclear palsy (PSP) syndrome and horizontal, gaze-evoked nystagmus (GEN), a finding hitherto assumed atypical for PSP[1].
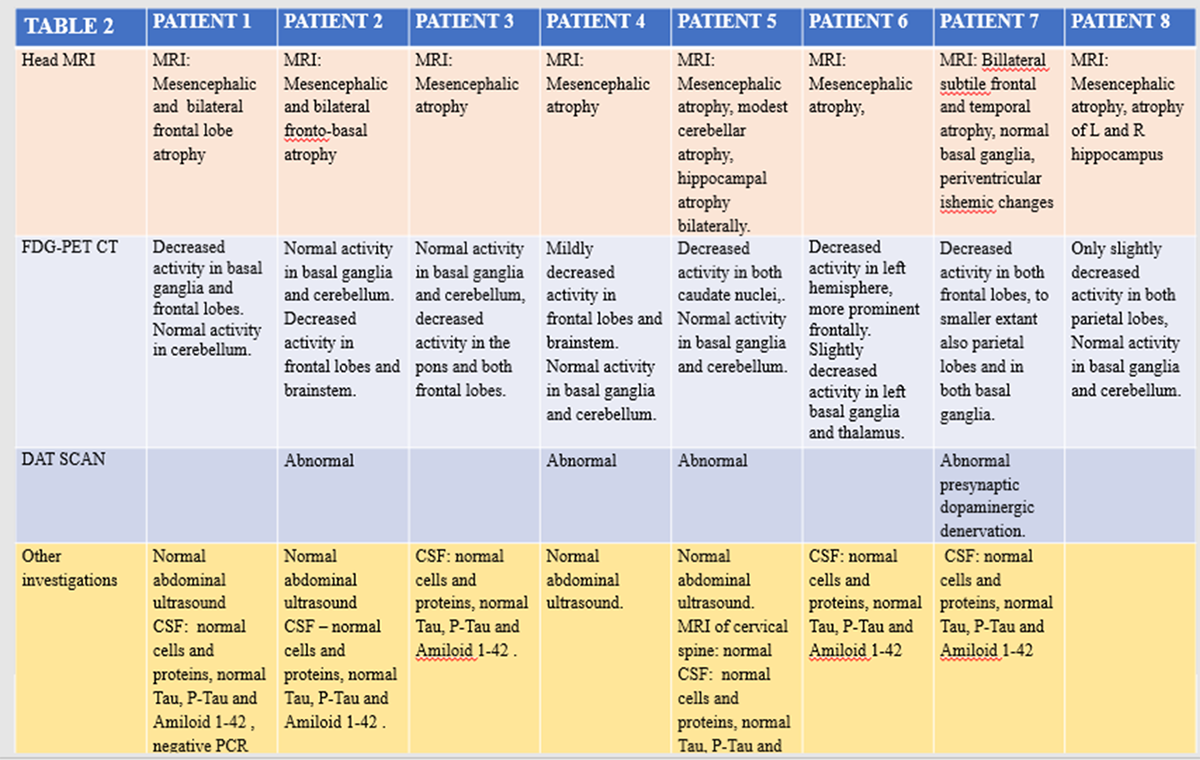
Background: The diagnosis of PSP was made according to clinical criteria and further support by typical brain MRI findings and characteristic changes on brain FDG PET CT.
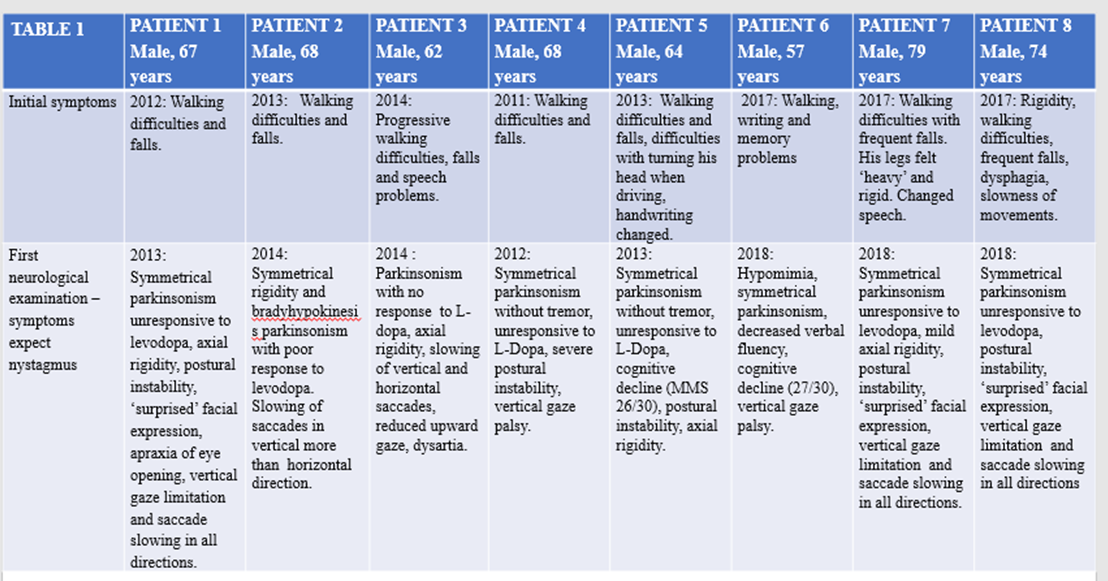
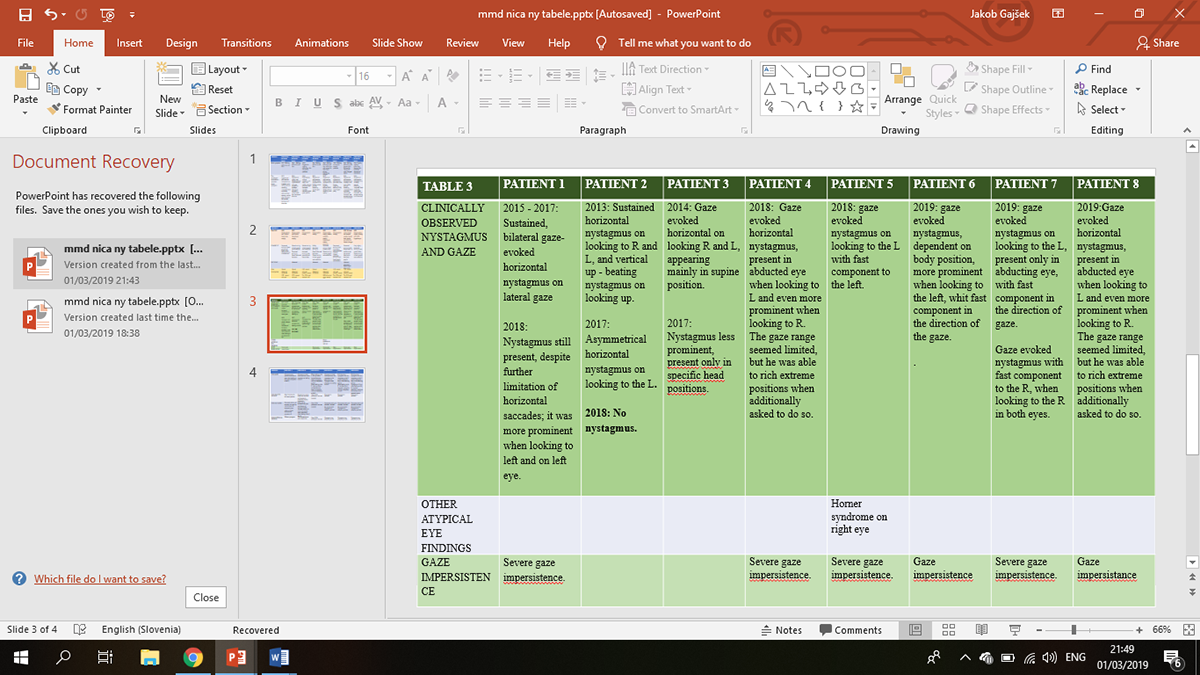
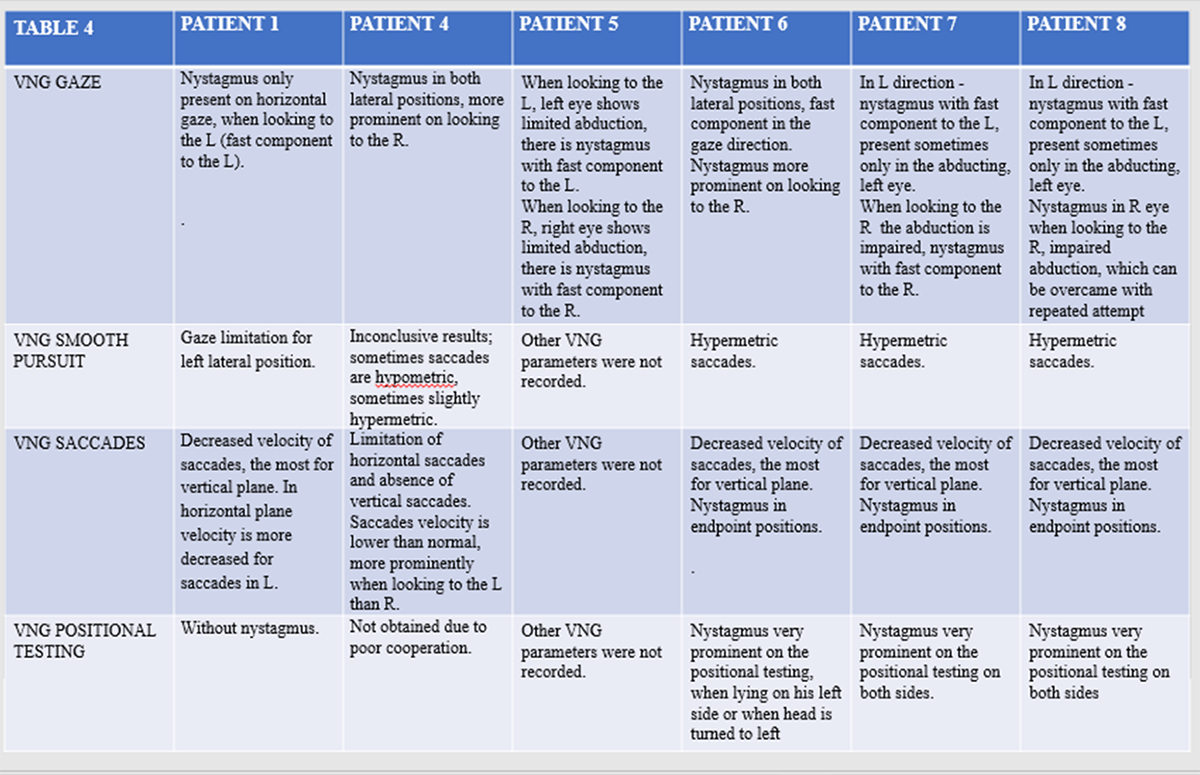
Method: Patients were clinically examined and videotaped [table 1,2,3,4]. Vestibulo-nystagmography was used for recording of the eye movements and the nystagmus. We searched pub med articles for previous descriptions of PSP patients with nystagmus.
Results: All patients with PSP syndrome had typical vertical gaze limitation and prominent slowing of vertical and horizontal saccades. In addition, they all showed horizontal GEN. Three different patterns of GEN could be differentiated: (i) GEN accompanying intranuclear ophthalmoplegia-like (INO)findings; (ii) GEN with lateral gaze impersistence and (iii) GEN present only in specific body positions. None of the patients had clinical or imaging signs of cerebellar dysfunction that could account for observed GEN. In the previous literature, we found only 4 single case reports of nystagmus in PSP[2,3,4,5].
Conclusion: The same pontine structures are responsible for both, the voluntary saccades and the fast phase of the nystagmus. Thus, it may be expected that slowing of the voluntary saccades is accompanied by loss of the fast component of the nystagmus, making the nystagmus atypical for PSP[6]. However, our observation suggests the GEN may be a part of abnormal oculomotor findings in PSP syndrome. GEN in PSP may arise as a consequence of frontal circuits for supranuclear voluntary saccadic control being disproportionally more affected than posterior cortical circuits, responsible for reflexive saccades. Asymmetrical brainstem neurodegeneration may contribute to GEN in the cases with INO-like findings. Finally, when nucleus prepositus hypoglossi, a part of horizontal gaze hoding system, is affected, a syndrome consisting of slowing of the saccades, nystagmus, vestibular disturbance and gaze impersistence may arise[8]. GEN is overlooked feature of PSP, probably as it only appears transiently, when horizontal saccades are not fully affected. Observing GEN should not deter the clinician from the diagnosis of PSP syndrome.
References: 1. Respondek G1, Kurz C, Arzberger T, et al. Which ante mortem clinical features predict progressive supranuclear palsy pathology? Movement Disorders. 2017;32:995-1005. 2. Koga S, Aoki N, Uitti RJ, et al. When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology. 2015;85:404-12.3. 3. Matsumoto H, Ohminami S, Goto J, Tsuji S. Progressive supranuclear palsy with wall-eyed bilateral internuclear ophthalmoplegia syndrome. Archieves of Neurology. 2008;65:827-9. 4. Gold DR, Atypical ocular motor features (gaze-evoked nystagmus) in PSP. Neuro-ophthalmology Virtual Education Library NOVEL. 2018;http://NOVEL.utah.edu. 5. Mastaglia FL,.Grainger KMR. Internuclear ophthalmoplegia in progressive supranuclear palsy Journal of the Neurological Sciences. Journal of the Neurological Sciences. 1975;25(3); 303-308. 6. Xu Z, Lim TCC, Au WL, Tan LCS. Progressive Supranuclear Gaze Palsy with Predominant Cerebellar Ataxia: A Case Series with Videos. Journal of Movement Disorders. 2017;10(2):87-91. doi:10.14802/jmd.1605 7. Kaneko CRS. Eye movement deficits after ibotenic acid lesions of the nucleus prepositus hypoglossi in monkeys. 1. Saccades and fixation. J Neurophysiol 1997;78:1753-68.
To cite this abstract in AMA style:
MK. Klarendic, MA. Hribar, SB. Battelino, MGK. Kramberger, MK. Kojovic. Gaze – evoked nystagmus in PSP patients: Is it really atiypical? A case series of eight patients [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/gaze-evoked-nystagmus-in-psp-patients-is-it-really-atiypical-a-case-series-of-eight-patients/. Accessed February 1, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/gaze-evoked-nystagmus-in-psp-patients-is-it-really-atiypical-a-case-series-of-eight-patients/