Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To determine the effect of sleep positions on morning OH in PD patients
Background: Orthostatic hypotension (OH) is considered one of the most disabling symptoms in Parkinson’s disease (PD) patients. Approximately half of the PD patients with OH have supine hypertension (SH) and nocturnal hypertension (NH), which are the major limitations of the effective treatment of OH. Sleeping positions are considered non-pharmacological treatments in patients with OH without worsening the SH and NH.
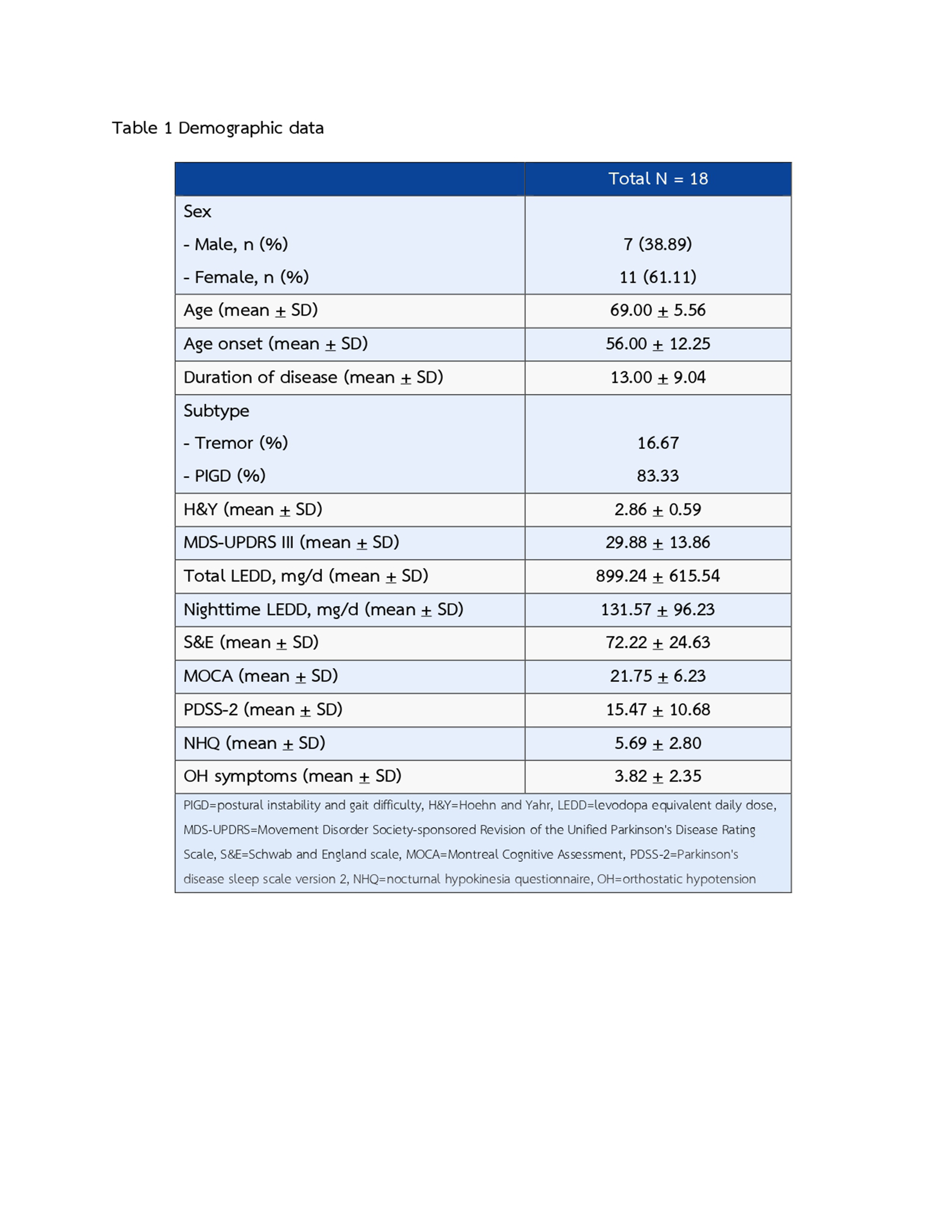
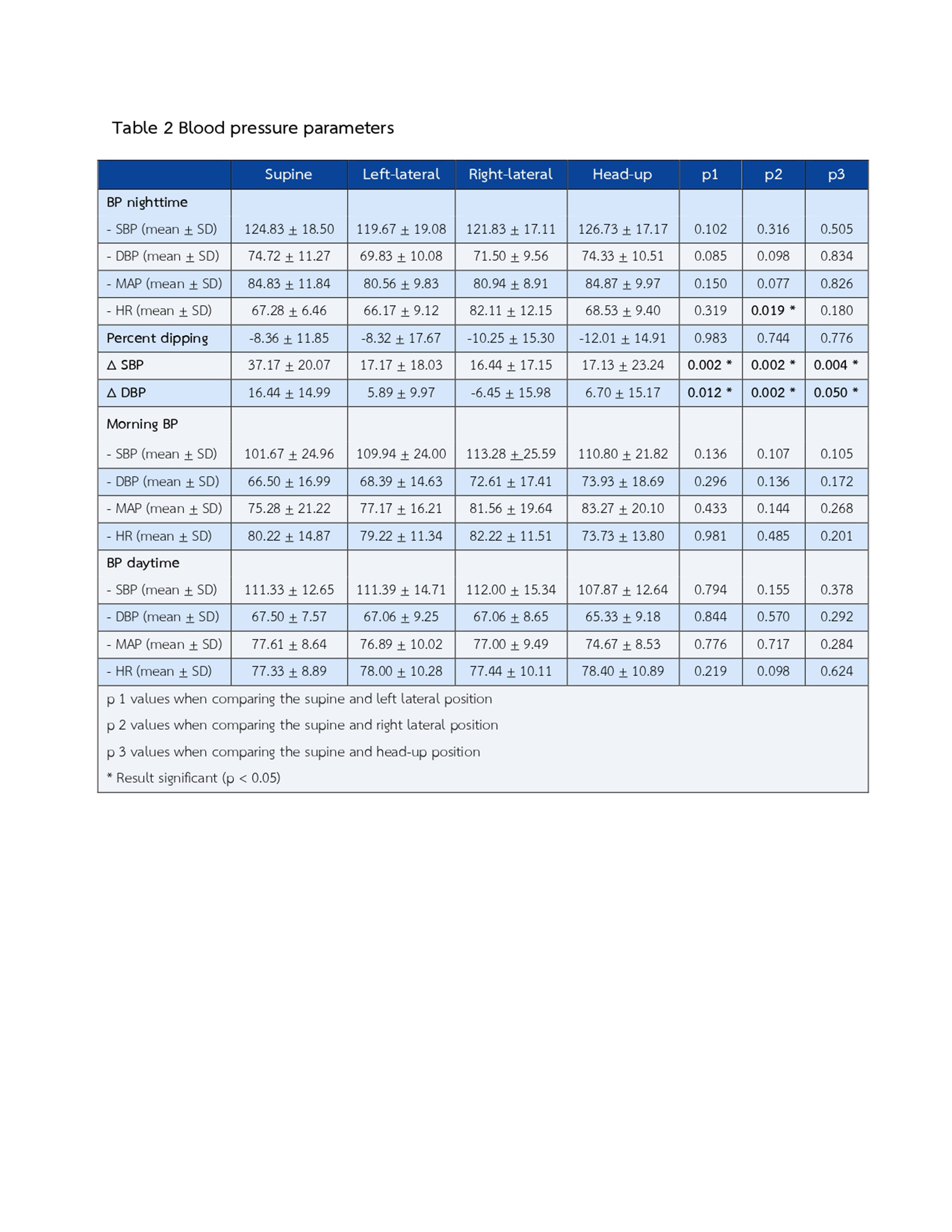
Method: This cross-sectional study enrolled 18 PD patients with OH. They were monitored 24-hours ambulatory blood pressure (ABPM) at home for four days and nights. Patients were instructed to sleep in the supine position for the entire first night as a baseline, then left lateral position, right lateral position, and 20-centimetres-head-up position for the entire second, third, and fourth night, respectively. The morning OH was assessed immediately after awakening.
Results: There were 7 males and 11 females with an average age of 69.00±5.56, and disease duration of 13.00±9.04 years. The mean of H&Y staging was 2.86±0.59. The mean daytime SBP and DBP at baseline were 115.33±12.81 and 69.78±6.90 mmHg, and the mean nighttime SBP and DBP at baseline were 124.83±18.50 and 72.72±11.27 mmHg, respectively. We found a statistically significant difference in morning OH magnitude between sleeping in the supine and lateral position, either left- and right-lateral position (supine ∆SBP vs. left-lateral ∆SBP: 37.17±20.07 vs. 17.17±18.03, p=0.002; supine ∆DBP vs. left-lateral ∆DBP: 16.44±14.99 vs. 5.89±9.97, p=0.012; supine ∆SBP vs. right-lateral ∆SBP: 37.17±20.07 vs. 16.44±17.15, p=0.002; supine ∆DBP vs. right-lateral ∆DBP: 16.44±14.99 vs. -6.45±15.98, p=0.002) and between supine and head-up position (supine ∆SBP vs. head-up ∆SBP: 37.17±20.07 vs. 17.13±23.24, p=0.004; supine ∆DBP vs. head-up ∆DBP: 16.44±14.99 vs. 6.70±15.17, p= 0.05), whereas, no statistically significant when compared both lateral positions and head-up positions.
Conclusion: Our study demonstrated the effect of sleeping position on morning OH in PD patients. We found a statistically significant difference of morning OH magnitude between sleeping in supine and lateral positions and sleeping in a head-up position. And thus, we proposed that lateral sleep position might be a novel non-pharmacological treatment for PD patients with OH in the morning.
References: – Palma JA, Kaufmann H. Orthostatic Hypotension in Parkinson Disease. Clin Geriatr Med. 2020;36(1):53-67.
– Espay AJ, LeWitt PA, Hauser RA, Merola A, Masellis M, Lang AE. Neurogenic orthostatic hypotension and supine hypertension in Parkinson’s disease and related synucleinopathies: prioritisation of treatment targets. The Lancet Neurology. 2016;15(9):954-66.
– Fanciulli A, Göbel G, Ndayisaba JP, Granata R, Duerr S, Strano S, et al. Supine hypertension in Parkinson’s disease and multiple system atrophy. Clin Auton Res. 2016;26(2):97-105.
– J. Sringean, R. Hamindra, Bhidayasiri R. The prevalence of supine hypertension and nocturnal hypertension and the difference of blood pressure in each sleep position in Parkinson’s disease [abstract]. Movement Disorders. 2019;34.
To cite this abstract in AMA style:
T. Prasertpan, R. Chokesuwattanaskul, J. Sringean, S. Siwanogsatham, R. Bhidayasiri. What is the appropriate sleep position for Parkinson’s disease patients with orthostatic hypotension in the morning? [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/what-is-the-appropriate-sleep-position-for-parkinsons-disease-patients-with-orthostatic-hypotension-in-the-morning/. Accessed July 3, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/what-is-the-appropriate-sleep-position-for-parkinsons-disease-patients-with-orthostatic-hypotension-in-the-morning/