Objective: To identify whether MDS-UPDRS scores, Dopamine Transporter (DaT) Striatal Binding Ratios (SBRs), or dopamine metabolites cerebrospinal fluid (CSF) concentrations could predict the likelihood of depressive episodes at 10-year follow up in participants with Parkinson’s Disease without depression at baseline.
Background: Depression in PD is associated with significant morbidity and increased caregiver burden [1]. Its pathophysiology is multifactorial, possibly involving multiple neurotransmitter systems and pathways [2]. Prior cross-sectional analyses have shown MDS-UPDRS and sex to be associated with depression in PD [3]. It is yet to be seen whether the MDS-UPDRS non-motor and motor severity scores can predict the development of depression or whether a combined prediction model with MDS-UPDRS scores, SBR, and dopamine metabolites would improve its accuracy.
Method: Logistic regression models were used to assess the predictive accuracy of MDS-UPDRS subsections scores, CSF dopamine metabolites, and DaT SBRs for the likelihood of presence of depression, defined as Geriatric Depression Scale-15 (GDS) >4, at any visit over a 10-year period in PD participants who did not have baseline depression (GDS <5). Welch’s t-test assessed baseline differences in demographics and MDS-UPDRS scores between participants with (PDw) or without suspected depression (PDwo) by 10-year follow up.
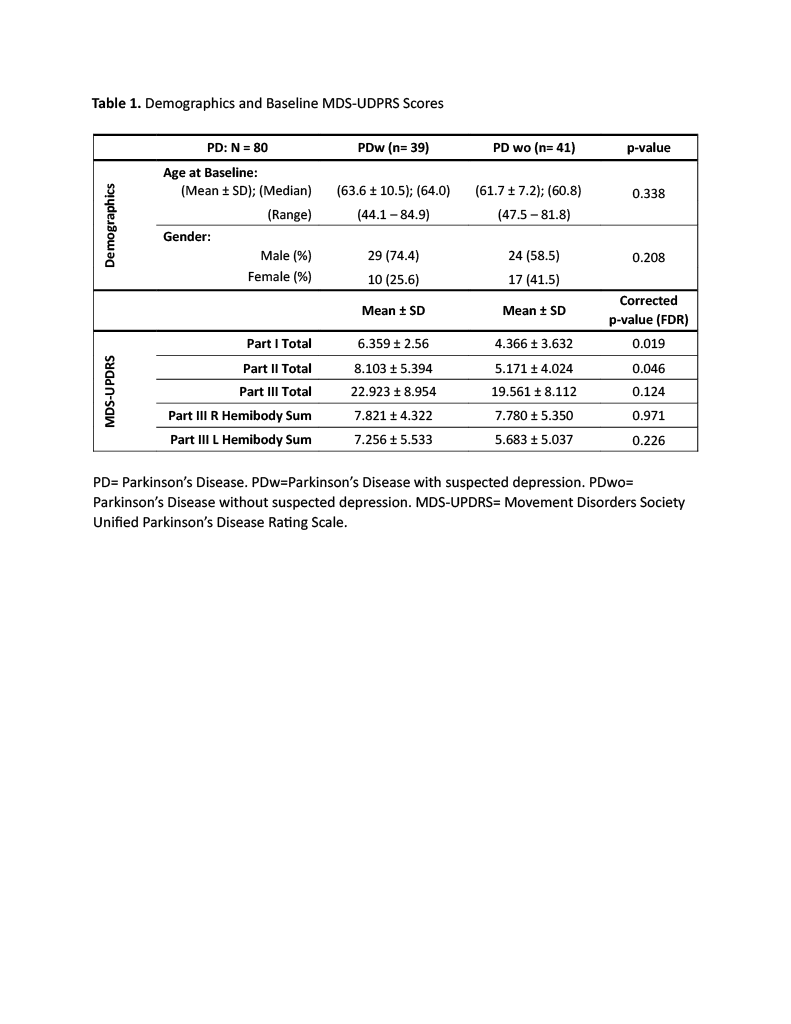
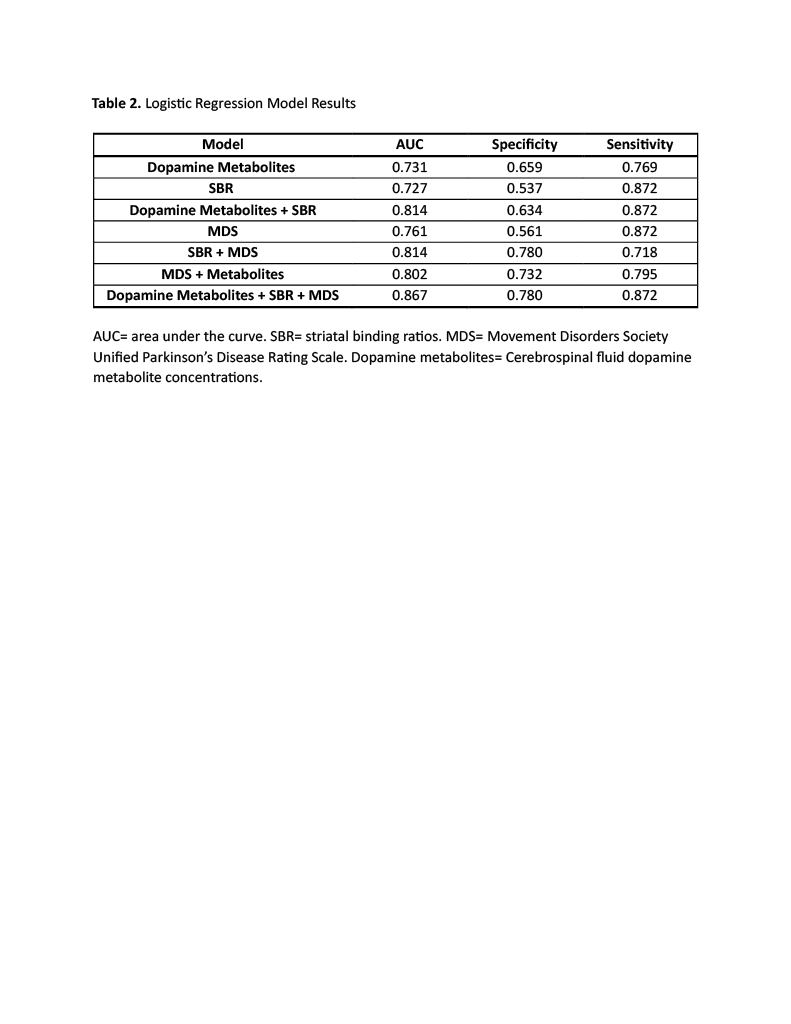
Results: PDw (n=39) had higher baseline MDS-UPDRS Part I and II, but not Part III scores compared to PDwo (n=41) (Table 1). The Logistic regression model found neither Parts I, II, or III were individually significant predictors of developing depression. Individually, all 3 measures achieved similar AUCs (MDS-UPDRS 0.76, dopamine metabolites 0.73, SBR 0.73). A combination of all 3 measures achieved the highest AUC (0.86) (Table 2).
Conclusion: Baseline MDS-UPDRS scores, CSF dopamine metabolite concentrations, and DaT SBRs achieved similar prediction accuracies for likelihood of developing depressive symptoms at 10-year follow up and all were “acceptable” [4]. The combination of all three measures achieved “excellent” accuracy [4]. There is potential overfitting of our models since our logistic regression models did not split data into training and test datasets and we had many predictor variables relative to the sample size.
Table 1
Table 2
References: 1. Brumm MC, Siderowf A, Simuni T, et al. Parkinson’s Progression Markers Initiative: A Milestone-Based Strategy to Monitor Parkinson’s Disease Progression. J Parkinsons Dis. 2023;13(6):899-916. doi:10.3233/JPD-223433
2. Prange S, Klinger H, Laurencin C, Danaila T, Thobois S. Depression in Patients with Parkinson’s Disease: Current Understanding of its Neurobiology and Implications for Treatment. Drugs Aging. 2022;39(6):417-439. doi:10.1007/s40266-022-00942-1
3. Sujith P, Arjunan P, Iype T, Natarajan V. Depression in Patients With Parkinson’s Disease: A Hospital-Based Cross-Sectional Study. Cureus. 2023;15(10):e47214. Published 2023 Oct 17. doi:10.7759/cureus.47214
4. Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315-1316. doi:10.1097/JTO.0b013e3181ec173d
To cite this abstract in AMA style:
J. Li, A. Basu, C. Song, I. Bedoy, J. Ruiz Tejeda, S. Nguyen, R. Rajmohan, N. Phielipp. Assessing the Accuracy of Clinical features, CSF Dopamine Metabolites, and Striatal Binding Ratios for the Likelihood of Depression Over 10-year Follow Up in the PPMI Cohort. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/assessing-the-accuracy-of-clinical-features-csf-dopamine-metabolites-and-striatal-binding-ratios-for-the-likelihood-of-depression-over-10-year-follow-up-in-the-ppmi-cohort/. Accessed March 5, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/assessing-the-accuracy-of-clinical-features-csf-dopamine-metabolites-and-striatal-binding-ratios-for-the-likelihood-of-depression-over-10-year-follow-up-in-the-ppmi-cohort/