Objective: Examine whether Parkinson’s disease patients (PD) who experience hallucinations (PD+hall) exhibit a greater decline in striatal dopamine and corresponding posterior cortical decline relative to PD patients without hallucinations (PD-ctrl).
Background: The development of visual hallucinations in PD is a significant predictor of dementia and earlier nursing home placement[1]. A reduction in striatal dopamine transporter has independently been linked to posterior cortical atrophy[2] and psychosis[3], [4].
Method: This study used data from a cohort of de novo PD patients and healthy controls (HC) enrolled in the Parkinson’s Progression Markers Initiative. We extracted longitudinal cortical thickness values from T1-weighted structural MRI and striatal binding ratios (SBRs) in the putamen and caudate from 123I-ioflupane SPECT data for 34 HC, 34 PD-ctrl, and 34 PD+hall matched on age, sex, education, and PD severity via Hoehn and Yahr score. Four 3 × 4 [group (PD+hall vs PD-ctrl) × Time (baseline, year 1, 2, and 4)] repeated measures analyses of variance were conducted with striatal SBR values as the dependent variables to examine whether SBRs exhibited a greater decline over time in the PD+hall relative to PD-ctrl groups. Additionally, general linear models were used to examine the relationship between SBRs and cortical thickness across time.
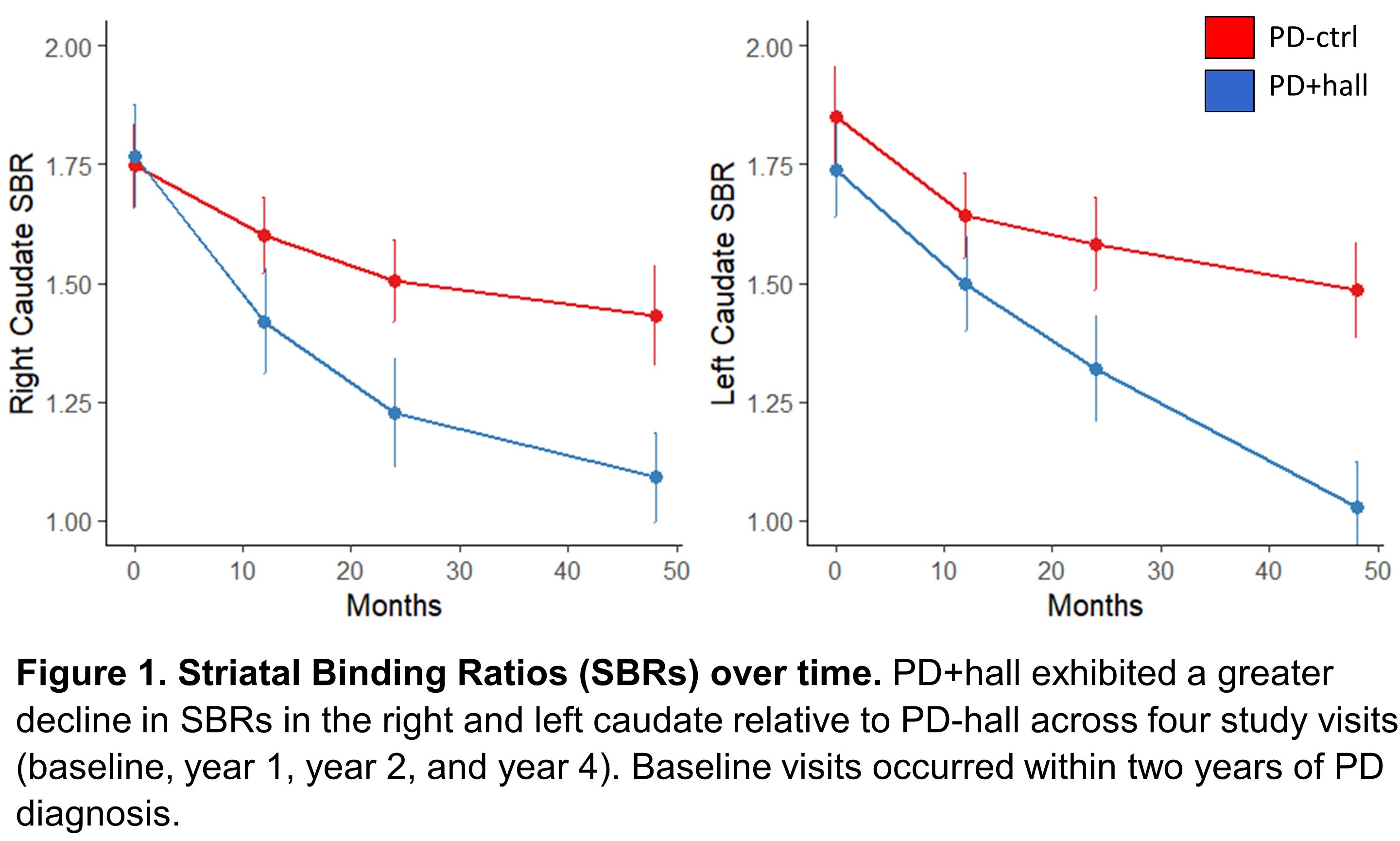
Results: PD+hall exhibited a greater reduction in SBR in the left and right caudate over time relative to PD-ctrl [figure 1]. A greater reduction in caudate SBR values was associated with reduced cortical thickness over time in the left lateral occipital (p = 0.01), right superior parietal (p = 0.001), and precentral gyri (p = 0.01) in the PD+hall group only. Lastly, reduced right putamen SBR was associated with cortical thinning in the PD+hall group in the right precentral gyrus (p = 0.04).
Conclusion: PD+hall exhibit a greater decline in striatal dopamine binding and associated posterior cortical thinning in the left lateral occipital, right superior parietal, and precentral gyri. This suggests dopamine degeneration may play role in posterior cortical thinning and the development of hallucinations. This work has previously been presented at the International Neuropsychological Society, February, 2021.
References: [1] D. Weintraub, P. J. Moberg, J. E. Duda, I. R. Katz, and M. B. Stern, “Effect of psychiatric and other nonmotor symptoms on disability in Parkinson’s disease,” J. Am. Geriatr. Soc., vol. 52, no. 5, pp. 784–788, 2004. [2] F. Sampedro, J. Marín-Lahoz, S. Martínez-Horta, J. Pagonabarraga, and J. Kulisevsky, “Dopaminergic degeneration induces early posterior cortical thinning in Parkinson’s disease,” Neurobiol. Dis., vol. 124, pp. 29–35, 2019. [3] E. Jaakkola, J. Joutsa, E. Mäkinen, J. Johansson, and V. Kaasinen, “Ventral striatal dopaminergic defect is associated with hallucinations in Parkinson’s disease,” Eur. J. Neurol., vol. 24, no. 11, pp. 1341–1347, 2017. [4] B. Ravina et al., “Dopamine transporter imaging is associated with long‐term outcomes in Parkinson’s disease,” Mov. Disord., vol. 27, no. 11, pp. 1392–1397, 2012.
To cite this abstract in AMA style:
C. Wertz, K. Poston, N. Shaff, A. Hartman, A. Horner, A. Mayer, A. Vakhtin, A. Deligtisch, S. Pirio Richardson, S. Ryman. Parkinson’s disease patients with hallucinations exhibit dopaminergic degeneration and cortical thinning [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/parkinsons-disease-patients-with-hallucinations-exhibit-dopaminergic-degeneration-and-cortical-thinning/. Accessed March 13, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/parkinsons-disease-patients-with-hallucinations-exhibit-dopaminergic-degeneration-and-cortical-thinning/