Objective: To identify the associations between Alzheimer Disease (AD) co-pathology and neuropsychiatric symptoms in Lewy body dementia (LBD).
Background: Dementia with Lewy Bodies (DLB) and Parkinson Disease Dementia, referred to as LBD, are neurodegenerative dementias with highly variable clinical presentations [1]. Approximately 50% of LBD patients have AD co-pathology on autopsy, and this co-pathology contributes to clinical heterogeneity [2,3]. However, neuropsychiatric symptom associations of AD co-pathology in LBD have not been extensively investigated. A small study including 27 DLB patients showed that AD co-pathology is associated with fewer delusions and hallucinations [4], and the other neuropsychiatric symptoms commonly seen in LBD and AD were not assessed.
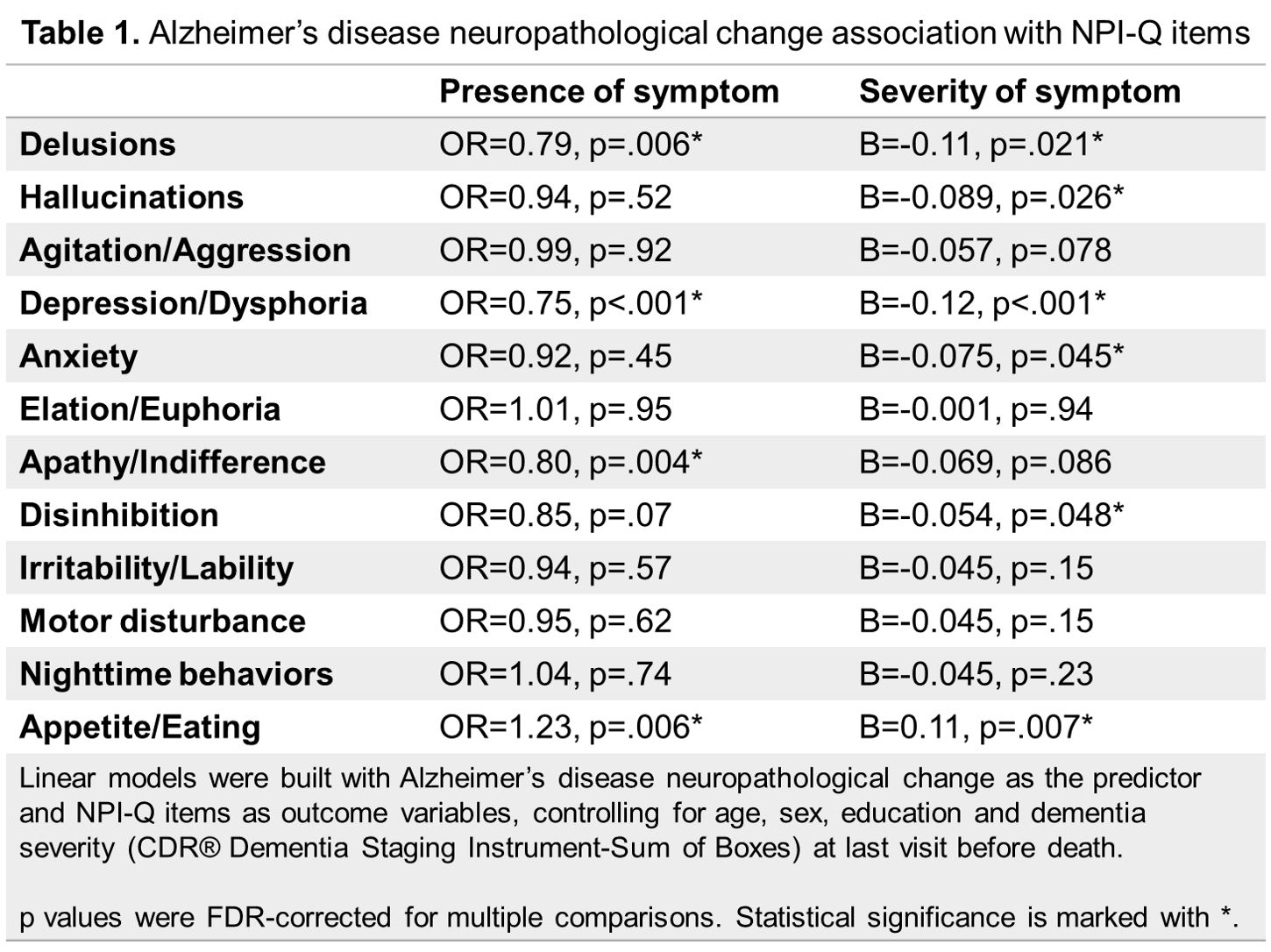
Method: Data was obtained from the National Alzheimer’s Coordinating Center Uniform Data Set (UDS) [5] and Neuropathology Data Set [6] for UDS visits conducted between September 2005 and August 2019 at 33 AD Research Centers. Only individuals clinically diagnosed with LBD at last visit with neuropathological confirmation were included (n=288). The association between AD neuropathological change (NIA-AA none, low/Braak tau 0-II=1; NIA-AA intermediate/Braak tau III-IV=2; NIA-AA high/Braak tau V-VI=3) and Neuropsychiatric Inventory-Questionnaire (NPI-Q) scores (for neuropsychiatric symptom presence and severity) was assessed with linear models controlling for age, sex, education and dementia severity (CDR® Dementia Staging Instrument-Sum of Boxes) at last visit before death. p values were FDR-corrected for multiple comparisons.
Results: More severe AD co-pathology was associated with lower total NPI-Q (B= -0.60, p= 0.013). Those with more severe AD co-pathology were less likely to have depression, delusion, apathy, and more likely to have appetite/eating changes. More severe AD co-pathology was associated with less severe hallucination, delusion, disinhibition, anxiety, depression and more severe appetite/eating changes.
[table1]
Conclusion: In this large, autopsy-validated cohort of LBD patients, AD co-pathology contributes to the presence and severity of neuropsychiatric symptoms in LBD. Further assessment of the neuropsychiatric features at LBD onset and during the course of the disease in pathologically validated samples can help better elucidate clinicopathological correlations and improve ante-mortem diagnostic accuracy in LBD.
References: 1. Jellinger KA, Korczyn AD. Are dementia with Lewy bodies and Parkinson’s disease dementia the same disease? BMC Med. 2018 Dec 6;16(1):34. 2. Coughlin DG, Hurtig HI, Irwin DJ. Pathological Influences on Clinical Heterogeneity in Lewy Body Diseases. Mov Disord. 2019 Jan 29;35(1):5–19. 3. Jellinger KA. Dementia with Lewy bodies and Parkinson’s disease-dementia: current concepts and controversies. J Neural Transm. 2018 Apr 8;125(4):615–50. 4. Del Ser T, Hachinski V, Merskey H, Munoz DG. Clinical and pathologic features of two groups of patients with dementia with Lewy bodies: Effect of coexisting Alzheimer-type lesion load. Alzheimer Dis Assoc Disord. 2001;15(1):31–44. 5. Besser L, Kukull W, Knopman DS, Chui H, Galasko D, Weintraub S, et al. Version 3 of the National Alzheimer’s Coordinating Center’s Uniform Data Set. Alzheimer Dis Assoc Disord. 2018 Oct;32(4):1. 6. Besser LM, Kukull WA, Teylan MA, Bigio EH, Cairns NJ, Kofler JK, et al. The Revised National Alzheimer’s Coordinating Center’s Neuropathology Form—Available Data and New Analyses. J Neuropathol Exp Neurol. 2018 Aug 1;77(8):717–26.
To cite this abstract in AMA style:
J. Dipane, D. Coughlin, E. Bayram. Association between Alzheimer’s disease co-pathology and neuropsychiatric symptoms in Lewy body dementia [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/association-between-alzheimers-disease-co-pathology-and-neuropsychiatric-symptoms-in-lewy-body-dementia/. Accessed July 10, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/association-between-alzheimers-disease-co-pathology-and-neuropsychiatric-symptoms-in-lewy-body-dementia/