Session Information
Date: Wednesday, June 7, 2017
Session Title: Parkinson's Disease: Psychiatric Manifestations
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To determine which baseline clinical symptoms are associated with future psychotic symptoms in de novo Parkinson disease (PD).
Background: Because psychosis in PD is associated with increased institutionalization, decreased quality of life, increased mortality, and greater caregiver burden, it is important to recognize early predictors of psychotic symptoms in PD.
Methods: This study evaluated a cohort of 423 newly diagnosed and untreated PD subjects collected as part of the Parkinson’s Progression Markers Initiative. PD symptoms were assessed at every visit using the Movement Disorders Society – Unified Parkinson Disease Rating Scale (MDS-UPDRS). Item 1.2 assesses hallucinations and psychosis over the past week. Any score greater than 0 indicated the presence of psychotic symptoms. At baseline, subjects completed a brief neuropsychological battery, the Geriatric Depression Scale, the Scales for Outcomes in Parkinson’s disease – Autonomic, the REM Sleep Behavior Disorder (RBD) Screening Questionnaire, and the Epworth Sleepiness Scale.
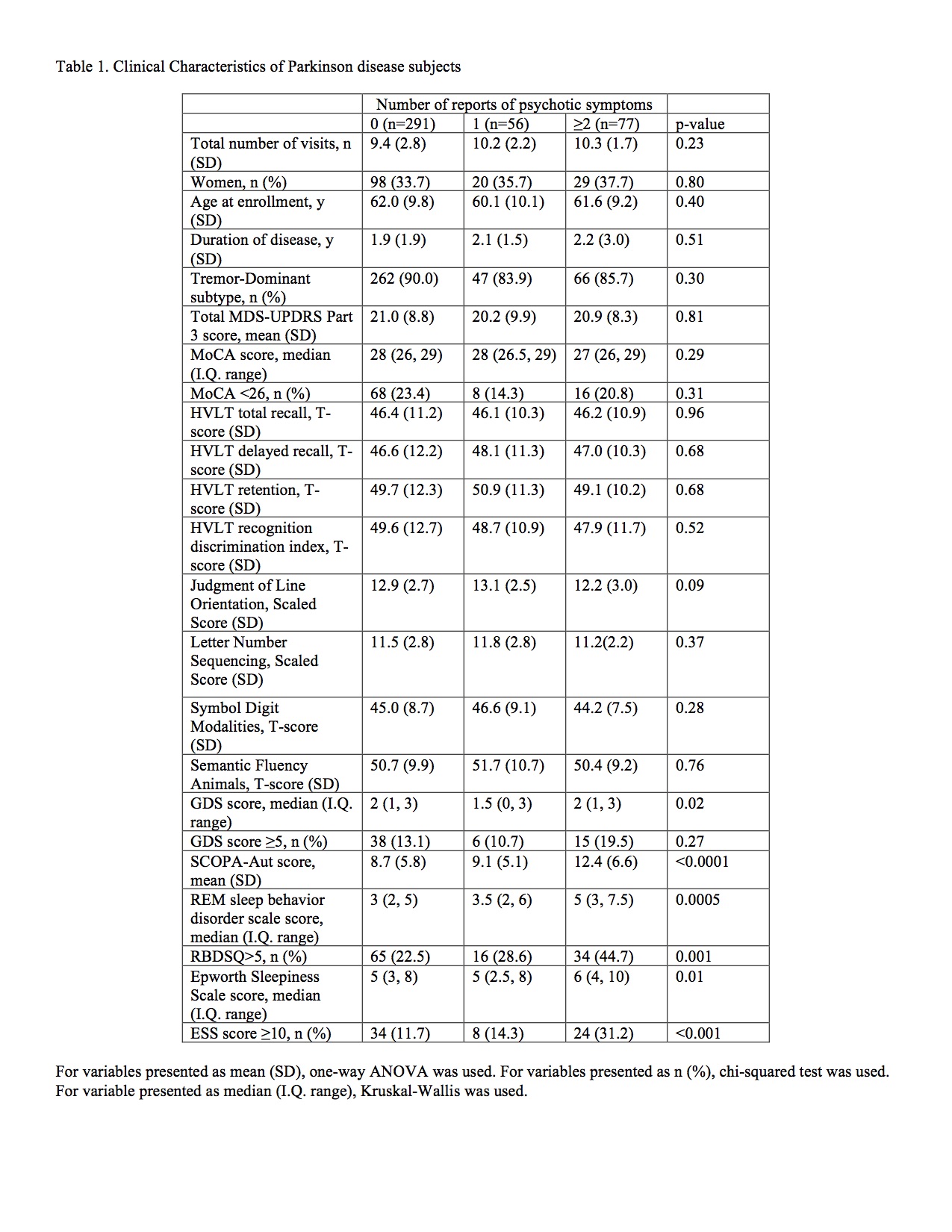
Results: The median number of visits per subject was 10 (I.Q. range: 11, 13) and the median last visit occurred 54 months after baseline (I.Q. range: 48, 60). For subjects who had their first psychotic event at some point prior to their last study visit, 85.7% (102/119) later reported no psychotic symptoms at at least one study visit. While no more than 16.1% (40/248) of subjects reported psychotic symptoms at any single study visit (48 month visit), 31.4% (133/423) of subjects reported psychotic symptoms at least once and 18.2% (77/423) reported psychotic symptoms more than once. [table1] Multivariate logistic regression adjusted for age and sex found that greater autonomic symptoms (OR=1.07 (for a 1-unit change in SCOPA); p=0.002), the presence of RBD (score ≥ 5) (OR=2.2, p=0.005), and excessive daytime somnolence (score≥10) (OR=2.39, p=0.006) at baseline were associated with increased risk of reporting psychotic symptoms on 2 or more occasions. In a similarly adjusted model, greater autonomic symptoms (OR=1.05; p=0.01), the presence of RBD (OR=1.9, p=0.03), and excessive daytime somnolence (OR=1.7, p=0.02) at baseline were associated with increased risk of psychotic symptoms on 1 or more occasions.
Conclusions: As reported in other studies, RBD, excessive daytime somnolence, and greater autonomic symptom burden are associated with greater risk of future psychotic symptoms in PD.
To cite this abstract in AMA style:
M. Barrett, M. Smolkin. Baseline Clinical Predictors of Future Psychotic Symptoms in de novo Parkinson Disease [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/baseline-clinical-predictors-of-future-psychotic-symptoms-in-de-novo-parkinson-disease/. Accessed March 4, 2026.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/baseline-clinical-predictors-of-future-psychotic-symptoms-in-de-novo-parkinson-disease/