Objective: To describe the process to create an interdisciplinary FND clinic with independent practitioners in the New York City area.
Background: Estimated 9,000 people in the New York metropolitan area are living with FND, with actual numbers possibly greater due under- and misdiagnosis common in this population. While an integrated approach has become the standard of care, a city-wide network of coordinated care is not yet established. Delays in cohesive, specialized treatment may negatively impact outcomes and recovery for people with FND.
Method: To describe our process to create a multi-institutional, interdisciplinary clinic and to report patient-encountered treatment barriers.
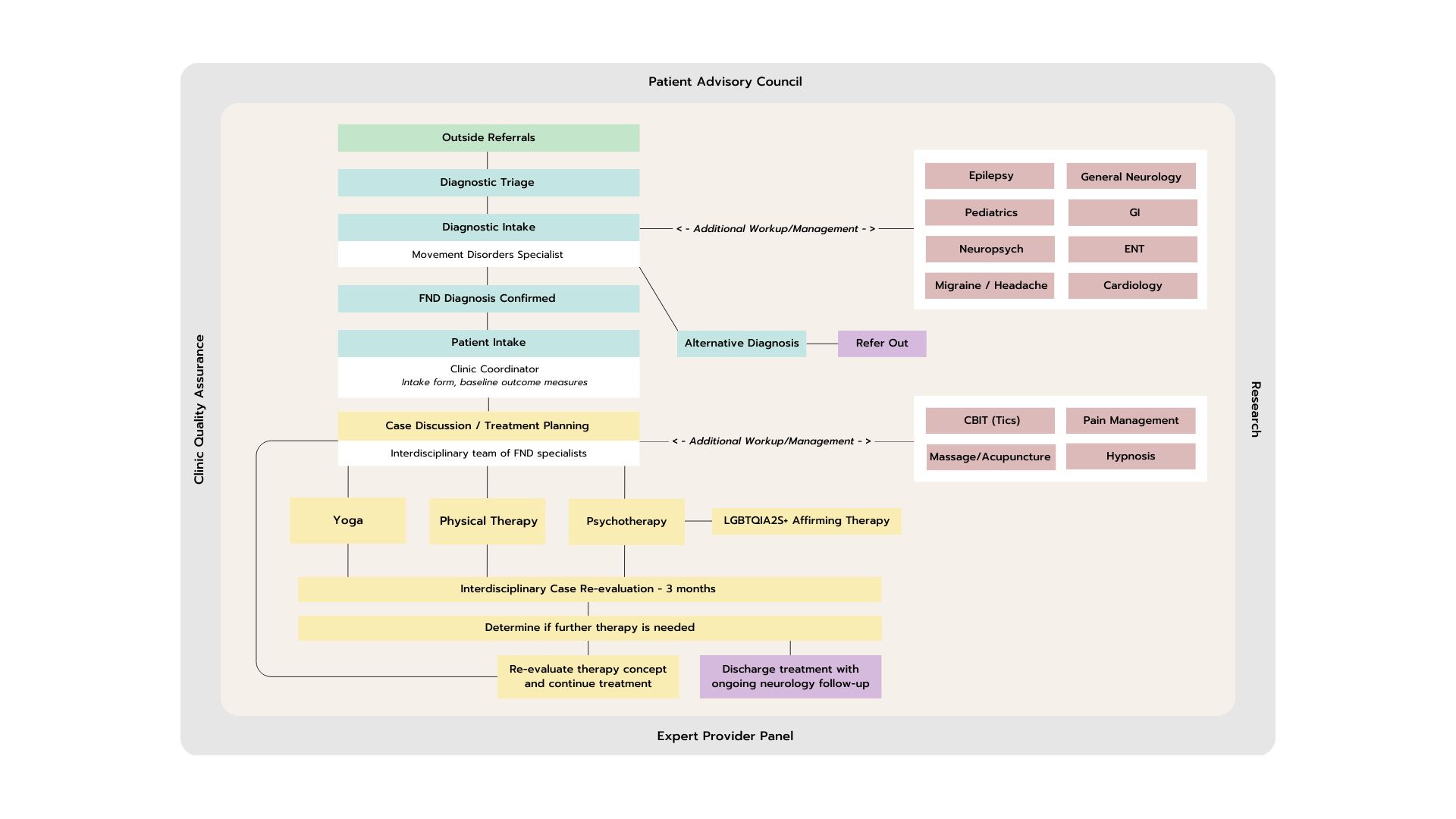
Results: To identify local FND providers, we individually searched a convenience sample of FND provider directories, professional websites, FND forums and social media platforms, and through patient word-of-mouth. We created a referral network of one neurologist, one dual-degree neurologist/social worker, one physical therapist, one yoga instructor, and one administrative assistant. We identified patient and community needs through unstructured interviews with pre-existing clients. We established bi-weekly meetings, an administrative structure, and an expert advisory panel consisting of neurologists, neuropsychologists, and physical therapists. To limit treatment gaps to marginalized communities, providers and staff participated in gender-affirming healthcare training. Based on shared clinical experience and administrative requirements, we created a formal clinic structure: (1) patient referral and intake, (2) bi-weekly case conferences, (3) consensus agreement on treatment decisions, (4) ongoing reevaluation until discharge from the clinic [fig. 1]. During case conferences, providers create a treatment plan based on individual patient needs and their own subspecialty expertise. Identified barriers to care include patient affordability and patient adherence to a multi-provider treatment plan. Future research will include statistical analysis of our patient population.
Conclusion: The creation of a community-based, interdisciplinary FND clinic is feasible in a populous and diverse city within the United States. We created a representative model of clinical care across institutions and private practices in Manhattan and Brooklyn. Further study is required to identify the benefits of this interdisciplinary model of care.
Figure 1
References: [1] M. Hallett, S. Aybek, B.A. Dworetzky, L. McWhirter, J.P. Staab, J. Stone, Functional neurological disorder: new subtypes and shared mechanisms, The Lancet Neurology 21 (2022) 537–550. https://doi.org/10.1016/S1474-4422(21)00422-1.
[2] S.C. Lidstone, L. MacGillivray, A.E. Lang, Integrated Therapy for Functional Movement Disorders: Time for a Change, Movement Disord Clin Pract 7 (2020) 169–174. https://doi.org/10.1002/mdc3.12888.
To cite this abstract in AMA style:
D. Kipnis, Z. Grin, S. Leung, Z. L'Erario, C. Amlang. Creating a Multi-institutional, Interdisciplinary Functional Neurological Disorder (FND) Clinic in an Urban Setting [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/creating-a-multi-institutional-interdisciplinary-functional-neurological-disorder-fnd-clinic-in-an-urban-setting/. Accessed July 15, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/creating-a-multi-institutional-interdisciplinary-functional-neurological-disorder-fnd-clinic-in-an-urban-setting/