Category: Parkinson's Disease: Neuroimaging
Objective: To explore MRI subcortical and cortical gray matter measures, as well as cognitive performance, in treated PD patients with REM sleep behavior disorder (RBD) symptoms.
Background: A few studies have shown that RBD is associated with cognitive impairment [1] and with decreased gray matter measures in PD patients when compared with PD patients without RBD, such as reduced thalamic [2], posterior cingulate, and hippocampus [3] volumes, and cortical thinning in perisylvian and inferior temporal cortices [4].
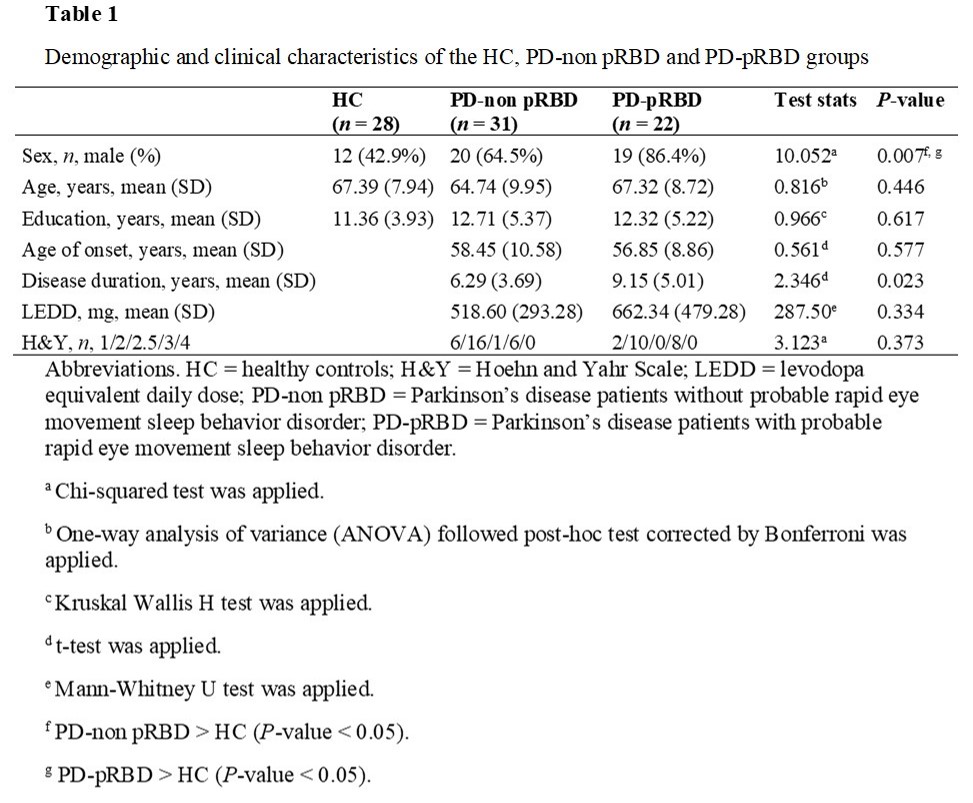
Method: The sample consisted of 53 PD patients from the Hospital Clinic of Barcelona classified according to the Innsbruck RBD Inventory into PD with probable RBD (PD-pRBD, n=22) and without probable RBD (PD-non pRBD, n=31) and 28 healthy controls. We performed between-group comparisons of global and subcortical segmentation, cortical thickness, and cognitive performance. The control group had more females than the PD groups, and the PD-pRBD group had more years of disease duration than the PD-non pRBD group [table1]. Then, these variables were used as covariates as required.The PD groups had no differences in motor severity.
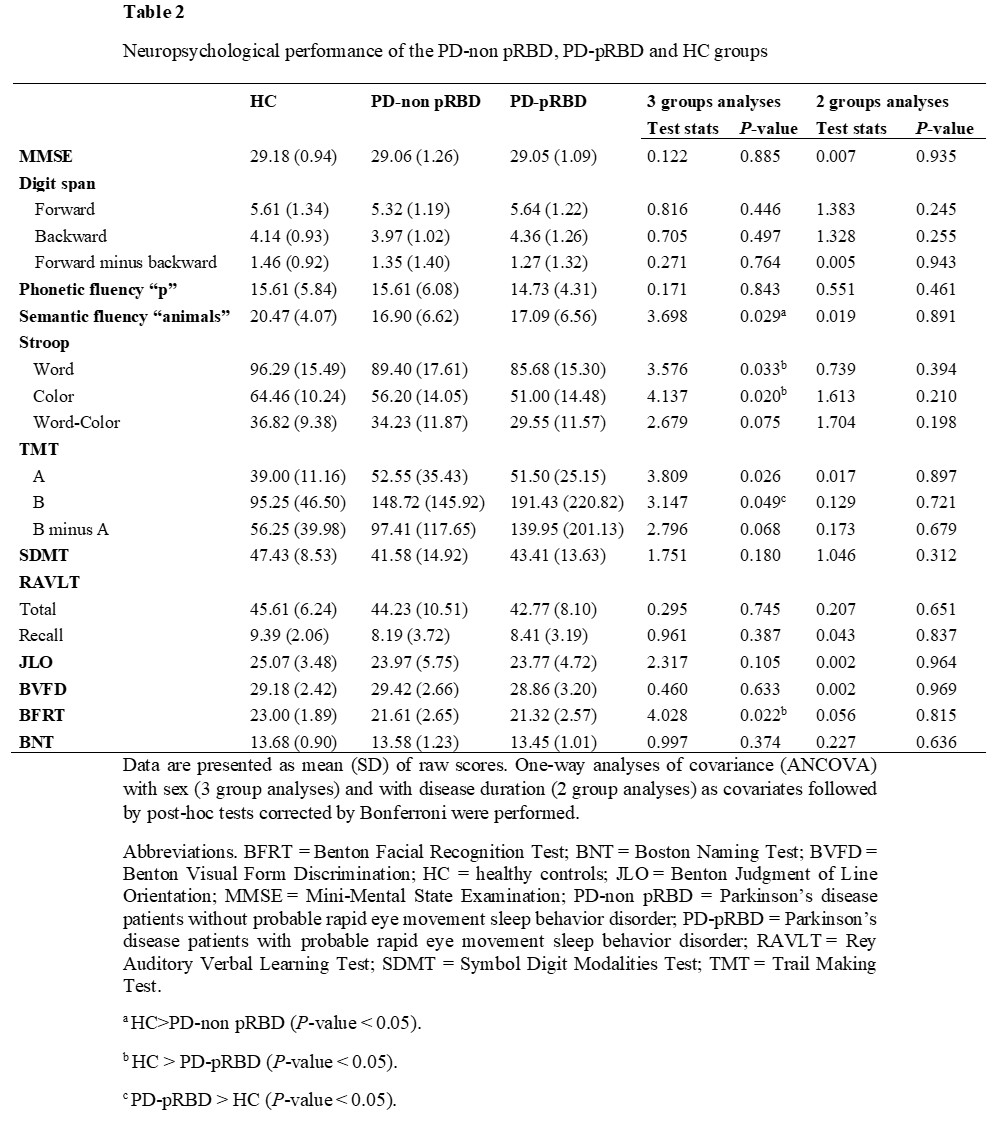
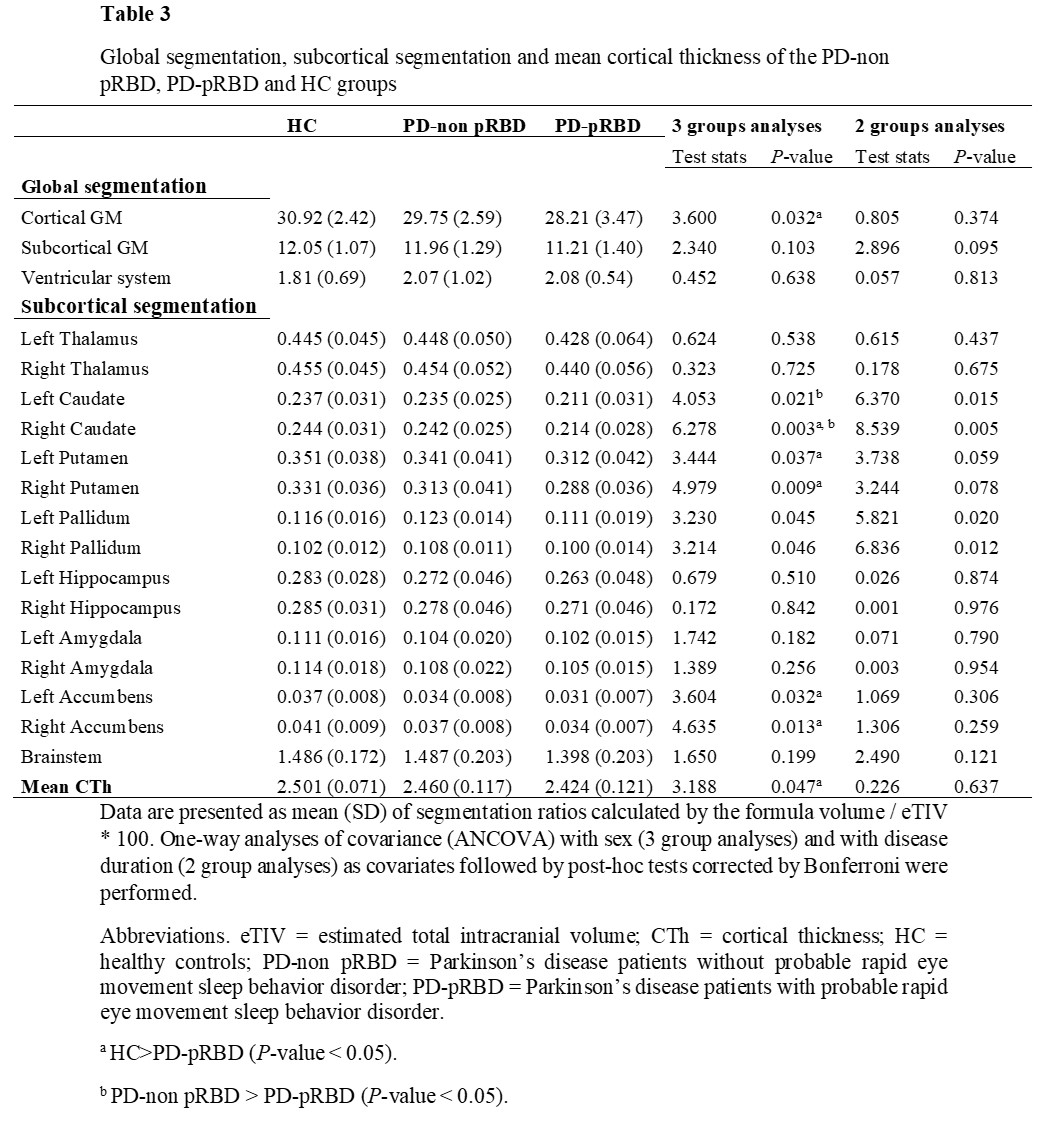
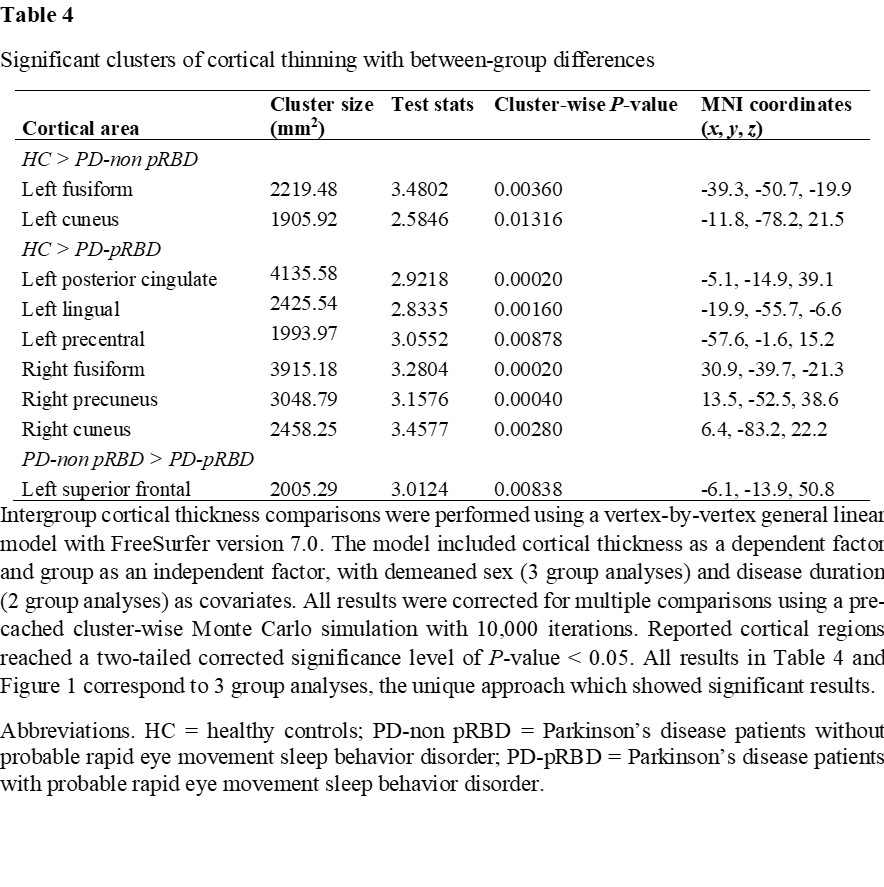
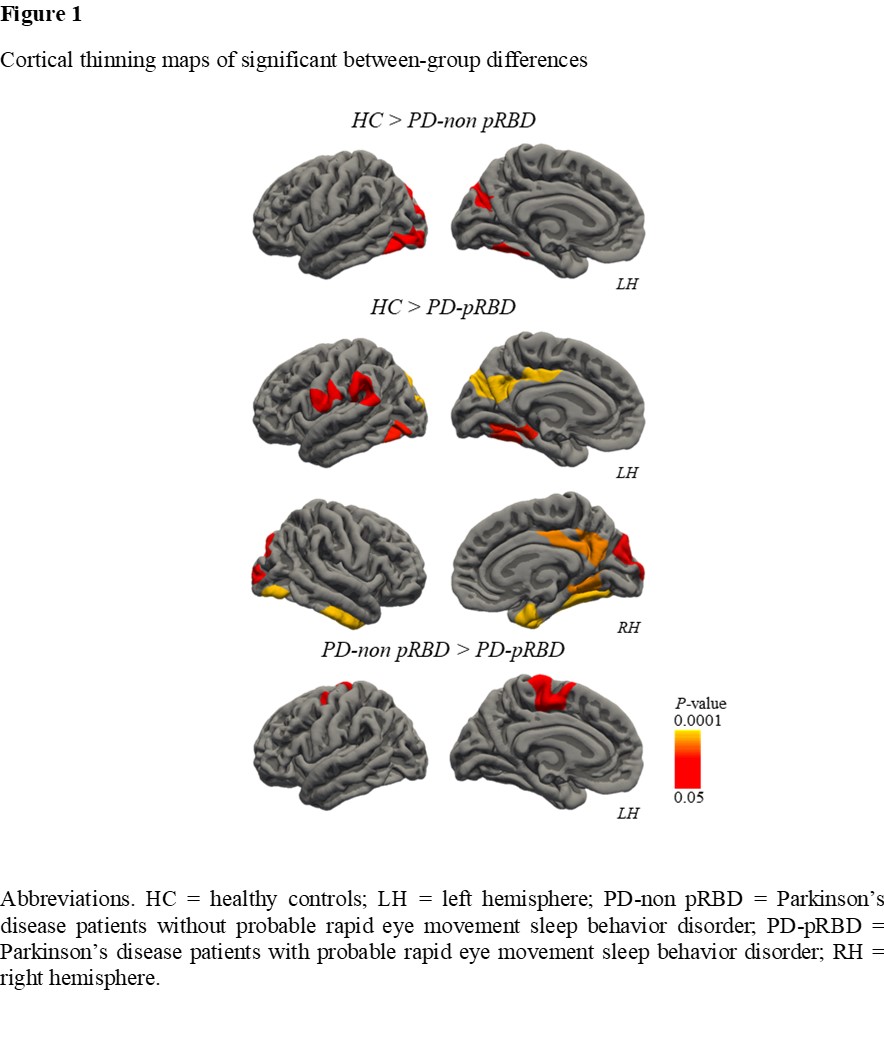
Results: The PD-pRBD group had worse performance than the control group in Stroop Word, Stroop Color, Trail Making Test B, and Benton Facial Recognition Test short form. The PD-non pRBD group had worse performance than the control group in semantic fluency [table2]. Concerning volumetric measures, PD-pRBD patients had decreased bilateral caudate and pallidum volumes compared with PD-non pRBD patients. Besides, PD-pRBD patients had decreased global cortical gray matter volume, right caudate, bilateral putamen, and bilateral accumbens volumes compared with controls [table3]. The PD-pRBD group had global cortical thinning compared with the control group [table3]. The PD-pRBD group had regional cortical thinning in the left superior frontal region compared with the PD-non pRBD group. As well as cortical thinning in the left posterior cingulate, left lingual, left precentral, right fusiform, right precuneus and right cuneus regions compared with the control group. The PD-non-pRBD group had regional cortical thinning in the left fusiform and left cuneus regions compared with the control group [table4, figure1].
Conclusion: Cognitive impairment and gray matter atrophy are more marked in PD patients with RBD symptomatology than without it.
References: 1. Lin Y. Q. & Chen S. D. RBD: a red flag for cognitive impairment in Parkinson’s disease?. Sleep Med. 2018; 44, 38–44. https://doi.org/10.1016/j.sleep.2018.01.006
2. Salsone M., Cerrasa A., Arabia G. et al. Reduced thalamic volume in Parkinson disease with REM sleep behavior disorder: volumetric study. Park. Relat. Disord. 2014; 20(9), 1004-1008. https://doi.org/10.1016/j.parkreldis.2014.06.012
3. Lim J. S., Shin S. A., Lee J. Y. et al. Neural substrates of rapid eye movement sleep behavior disorder in Parkinson’s disease. Park. Relat. Disord. 2016; 23, 31–36. https://doi.org/10.1016/j.parkreldis.2015.11.027
4. Rahayel S., Gaubert M., Postuma R. B. et al. Brain atrophy in Parkinson’s disease with polysomnography-confirmed REM sleep behavior disorder. Sleep 2019; 42(6), zsz062. https://doi.org/10.1093/sleep/zsz062
To cite this abstract in AMA style:
J. Oltra, A. Campabadal, C. Uribe, J. Pardo, MJ. Marti, Y. Compta, F. Valldeoriola, N. Bargallo, A. Iranzo, C. Junque, B. Segura. Gray matter volumetry, cortical thickness and cognitive performance in treated Parkinson’s disease with REM sleep behavior disorder symptomatology [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/gray-matter-volumetry-cortical-thickness-and-cognitive-performance-in-treated-parkinsons-disease-with-rem-sleep-behavior-disorder-symptomatology/. Accessed February 9, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/gray-matter-volumetry-cortical-thickness-and-cognitive-performance-in-treated-parkinsons-disease-with-rem-sleep-behavior-disorder-symptomatology/