Objective: To characterize LBD clinical subgroups and identify possible differences in disease progression.
Background: Patients with Lewy body disease (LBD) present a wide variety of symptoms resulting in clinical heterogeneity and different subgroups [1,2].
Method: We selected a longitudinal cohort of 454 LBD patients diagnosed with MCI or mild dementia (CDR 0.5 or 1) from National Alzheimer´s Coordinating Center database (NIA/NIH Grant: U24-AG072122).
A data-driven approach was applied using a factor analysis of mixed data (FAMD) and hierarchical cluster analysis. FAMD was used to reduce data dimensionality and identify dimensions based on demographic characteristics (age, sex, years of education, and disease duration), core features (parkinsonism, visual hallucinations, REM sleep behavior disorder (RBD), and fluctuating cognition), and cognitive variables (Mini-mental State Examination (MMSE) and neuropsychological performance). Hierarchical clustering analysis allowed us to identify clinical subtypes based on FAMD dimensions. Then, we applied a linear mixed-effects model to analyze disease progression rates across clusters during 5 years of follow-up using MMSE.
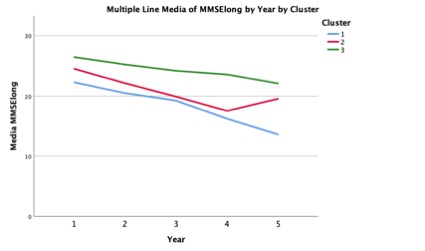
Results: We identified 3 clinical subgroups. Patients in cluster 1 were the oldest and more frequently female. This cluster had the lowest frequency of RBD and fluctuating cognition, demonstrated worse global cognition and semantic fluency than cluster 3, and had worse performance in language than cluster 2. Cluster 2 presented the highest frequency of RBD, parkinsonism, and fluctuating cognition, as well as more males. Cluster 3 had the highest level of education and the best performance in attention. There was no association between cluster and decrease in MMSE per year, after adjusting for age at baseline and years of education [figure1].
Conclusion: Patients with LBD can be classified in different clinical subgroups that present similar disease progression rates. A possible implication of these results in clinical practice is the increased risk of misdiagnosis in the cluster with less frequency of core features (cluster 1). Future studies should investigate potential differences in treatment response, and the influence of copathology in disease progression among LBD clinical subgroups.
References: 1. Lawton M, Ben-Shlomo Y, May MT, Baig F, Barber TR, Klein JC, et al. Developing and validating Parkinson’s disease subtypes and their motor and cognitive progression. J Neurol Neurosurg Psychiatry. 2018;89(12):1279–87.
2. Abdelnour C, Ferreira D, van de Beek M, Cedres N, Oppedal K, Cavallin L, et al. Parsing heterogeneity within dementia with Lewy bodies using clustering of biological, clinical, and demographic data. Alzheimer’s Res Ther. 2022;14(1):1–13.
To cite this abstract in AMA style:
C. Abdelnour, C. Young, E. Müller-Oehring, D. Ferreira, M. Shahid, M. Plastini, J. Winer, K. Poston. Lewy body disease clinical subgroups present similar disease progression rates [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/lewy-body-disease-clinical-subgroups-present-similar-disease-progression-rates/. Accessed July 1, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/lewy-body-disease-clinical-subgroups-present-similar-disease-progression-rates/