Category: Epidemiology
Objective: To assess the relationships of long-term blood pressure (BP) measures and incident Parkinson’s disease (PD) in the Framingham Heart Study (FHS) cohort.
Background: Long-term BP measures are indicators of cardiovascular (CV) risk, and CV risk factors are implicated in the development of PD [1-7]. Autonomic dysfunction occurs in PD, with worsening orthostatic hypotension and blood pressure variability (BPV) in later disease and is associated with greater white matter disease burden and motor dysfunction. Early autonomic dysfunction can also occur in prodromal and early PD [8-14]. FHS is a multigenerational longitudinal cohort study that was started in 1948, which is well-known for its extensive CV health data. In this study, we assessed the relationship of long-term BP measures and incident PD.
Method: Participants in the FHS Original and Offspring cohorts were included in this case-control study. Controls (HC) were selected based on sex, age on PD onset and FHS cohort with a 1:4 case-control ratio. Data was assessed over a 30-year period, and participants attended at least three health visits. BPV is assessed for both systolic (SBP) and diastolic blood pressures (DBP) using three metrics: 1) standard deviation, 2) adjusted cumulative blood pressure and 3) trajectory over time. Student’s t-test was used to assess each BPV metrics between cases and controls. Results were also weighted by number of examinations attended for each participant. PD diagnoses were made by a panel of movement disorders neurologists using the UK Brain Bank Criteria and other supporting clinical details. We used p<0.05 for significance.
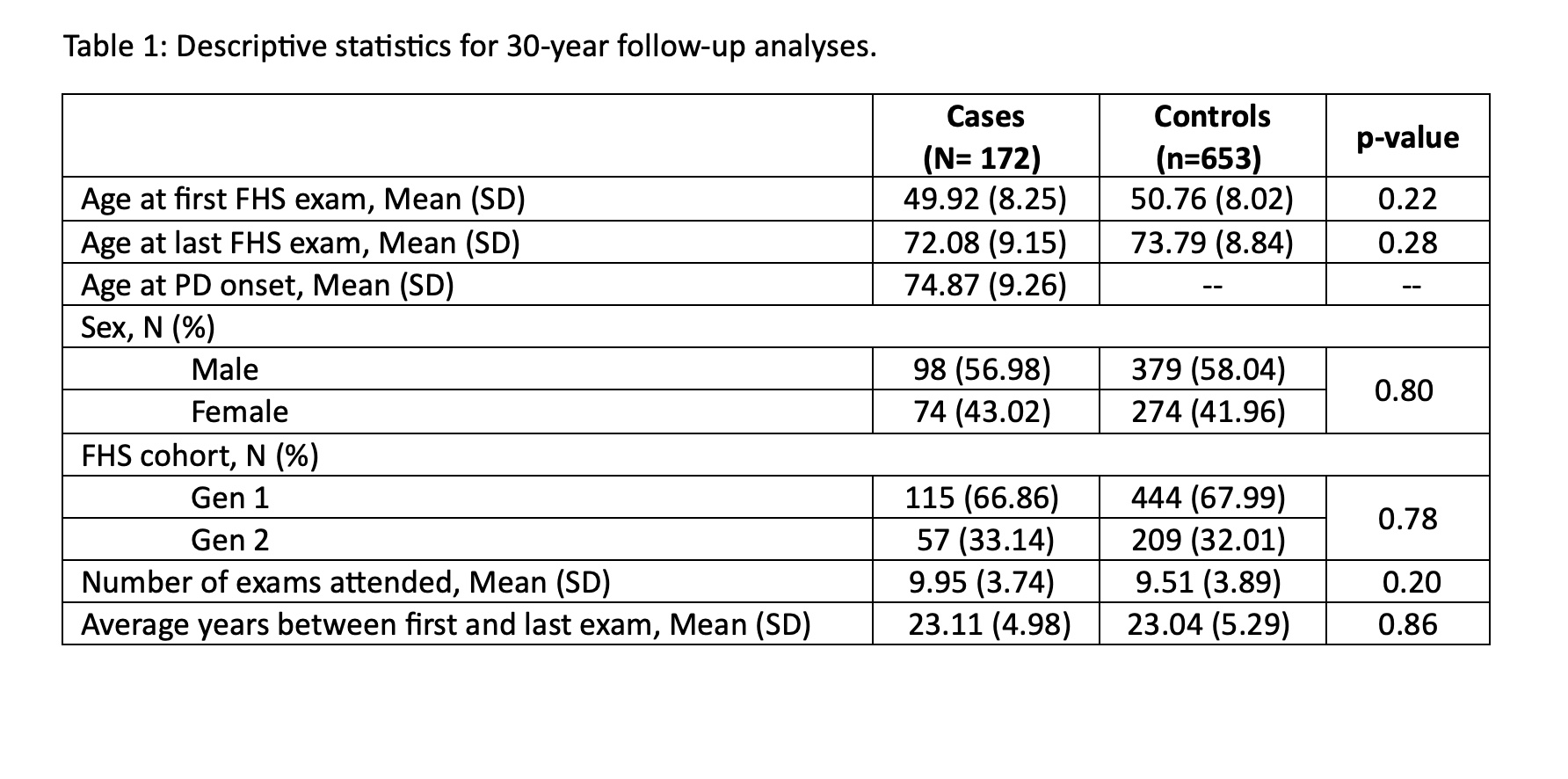
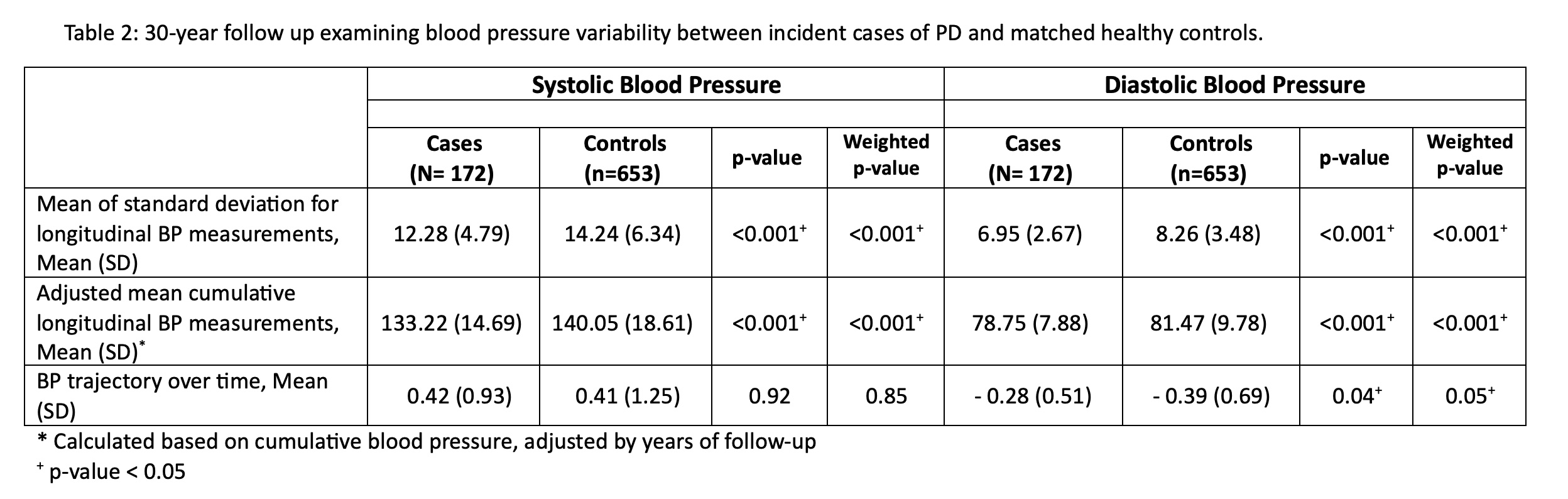
Results: A total of 172 PD cases (57% male) and 653 HC (58% male) were included in the analyses, average age of PD onset was 74.9 years. The meanage between first and last examination was approximately 23 years for both groups (Table 1). The mean standard deviation (STD) for longitudinal SBP was 12.28 (4.79) for cases and 14.24 (6.34) for HC (p <0.001). Mean STD for longitudinal DBP was 6.95 (2.67) and 8.26 (3.48) for HC, p <0.001.
Conclusion: Over time, participants who developed PD had less BPV compared to HC, which suggests that PD participants in this cohort may not have prodromal autonomic dysfunction. PD participants also had significantly lower absolute SBP compared to HC. Future analyses will use regression modeling to confirm these findings.
Table 1
Table 2
References: References:
1. Mehlum M.H., Liestøl K., Kjeldsen S.E., et al. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur. Heart J. 2018;39(24):2243–2251.
2. Rosei E.A., Chiarini G., Rizzoni D. How important is blood pressure variability? Eur. Heart J. Suppl. 2020;22(Supplement_E):E1–E6. doi: 10.1093/eurheartj/suaa061.
3. Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, McManus RJ. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016 Aug 9;354:i4098. doi: 10.1136/bmj.i4098. PMID: 27511067; PMCID: PMC4979357.
4. Schrag A, Bohlken J, Dammertz L, et al. Widening the Spectrum of Risk Factors, Comorbidities, and Prodromal Features of Parkinson Disease. JAMA Neurol. 2023;80(2):161–171. doi:10.1001/jamaneurol.2022.3902
5. Potashkin J, Huang X, Becker C, Chen H, Foltynie T, Marras C. Understanding the links between cardiovascular disease and Parkinson’s disease. Mov Disord. 2020 Jan;35(1):55-74. doi: 10.1002/mds.27836. Epub 2019 Sep 4. PMID: 31483535; PMCID: PMC6981000.
6. Hu G, Jousilahti P, Nissinen A, Antikainen R, Kivipelto M, Tuomilehto J. Body mass index and the risk of Parkinson disease. Neurology. 2006;67(11):1955-1959.
7. Hou L, Li Q, Jiang L, Qiu H, Geng C, Hong JS, Li H, Wang Q. Hypertension and Diagnosis of Parkinson’s Disease: A Meta-Analysis of Cohort Studies. Front Neurol. 2018 Mar 19;9:162. doi: 10.3389/fneur.2018.00162. PMID: 29615961; PMCID: PMC5867351.
8. Caminiti G., D’Antoni V., Morsella V., et al. Correlation between systolic blood pressure variability and global longitudinal strain in patients with Parkinson’s disease and dysautonomia. J. Cardiovasc. Dis. Res. 2020;11(1):1–3. doi: 10.5530/JCDR.2020.11.01.
9. Kotagal V, Albin RL, Müller ML, Koeppe RA, Frey KA, Bohnen NI. Modifiable cardiovascular risk factors and axial motor impairments in Parkinson disease. Neurology. 2014 Apr 29;82(17):1514-20. doi: 10.1212/WNL.0000000000000356. Epub 2014 Mar 28. PMID: 24682965; PMCID: PMC4011463.
10. Zhang B, Huo Y, Yang Z, Lv H, Wang Y, Feng J, Han Y, Wang H. Day to Day Blood Pressure Variability Associated With Cerebral Arterial Dilation and White Matter Hyperintensity. Hypertension. 2022 Jul;79(7):1455-1465. doi: 10.1161/HYPERTENSIONAHA.122.19269. Epub 2022 May 3. PMID: 35502669; PMCID: PMC9172904.
11. Goldstein DS, Eldadah BA, Holmes C, Pechnik S, Moak J, Saleem A, Sharabi Y. Neurocirculatory abnormalities in Parkinson disease with orthostatic hypotension: independence from levodopa treatment. Hypertension. 2005 Dec;46(6):1333-9. doi: 10.1161/01.HYP.0000188052.69549.e4. Epub 2005 Oct 10. PMID: 16216982.
12. Alves M, Caldeira D, Ferreira JJ. Blood pressure variability in Parkinson’s Disease patients – Case control study. Clin Park Relat Disord. 2023 Mar 1;8:100191. doi: 10.1016/j.prdoa.2023.100191. PMID: 36908283; PMCID: PMC9995452.
13. Postuma RB, Aarsland D, Barone P, Burn DJ, Hawkes CH, Oertel W, Ziemssen T. Identifying prodromal Parkinson’s disease: pre-motor disorders in Parkinson’s disease. Mov Disord. 2012 Apr 15;27(5):617-26. doi: 10.1002/mds.24996. PMID: 22508280.
14. Dommershuijsen LJ, Heshmatollah A, Mattace Raso FUS, Koudstaal PJ, Ikram MA, Ikram MK. Orthostatic Hypotension: A Prodromal Marker of Parkinson’s Disease? Mov Disord. 2021 Jan;36(1):164-170. doi: 10.1002/mds.28303. Epub 2020 Sep 23. PMID: 32965064; PMCID: PMC7891584.
To cite this abstract in AMA style:
S. O'Shea, Y. Liu, Y. Li, A. Gurnani, J. Dookhy, S. Frank, R. Au, J. Mez, T. Ang, L. Shih. Long-term Blood Pressure Measures in Incident Parkinson’s Disease in the Framingham Heart Study. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/long-term-blood-pressure-measures-in-incident-parkinsons-disease-in-the-framingham-heart-study/. Accessed July 15, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/long-term-blood-pressure-measures-in-incident-parkinsons-disease-in-the-framingham-heart-study/