Category: Other
Objective: To determine whether a Parkinson’s disease (PD) Inpatient Program will prevent medication errors and ultimately improve the safety and quality of care for hospitalized people with PD.
Background: Medication errors among hospitalized individuals with PD are associated with increased re-admission, 90-day mortality, and longer length of stay as demonstrated by our retrospective study [1]. In collaboration with the Parkinson’s Foundation, we designed a multidisciplinary proactive inpatient intervention.
Method: From January to June 2023, patients with a history of PD or primary parkinsonism were prospectively listed in a census built with a custom electronic health record (EHR) tool during their hospital admission at Cleveland Clinic Main Campus. The multidisciplinary approach consisted of 1) active intervention (review of the inpatient orders mirroring the stable outpatient regimen, checking for contraindicated medications, promoting early mobilization and periodic swallow screening, providing in-person and virtual consultation services when needed); 2) Staff education; 3) EHR changes (alerts for selected contraindicated medications); 4) pharmacist ensuring the accuracy of PD medication administrations particularly in cases where substitutions were required. Medication administration results during the 2023 intervention were compared to our retrospective 2018 data.
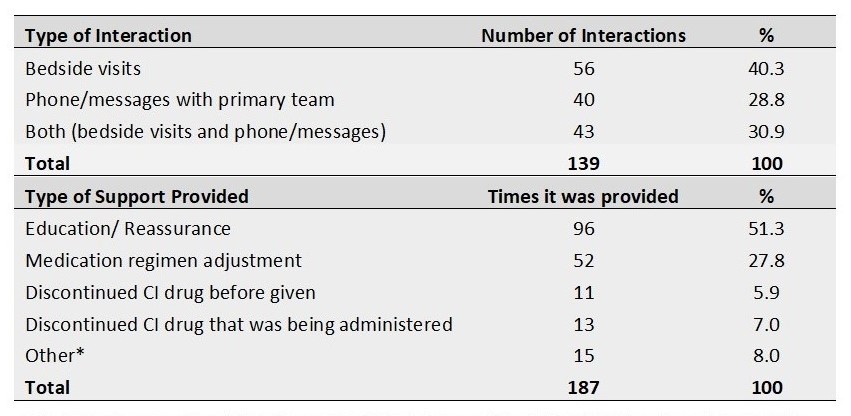
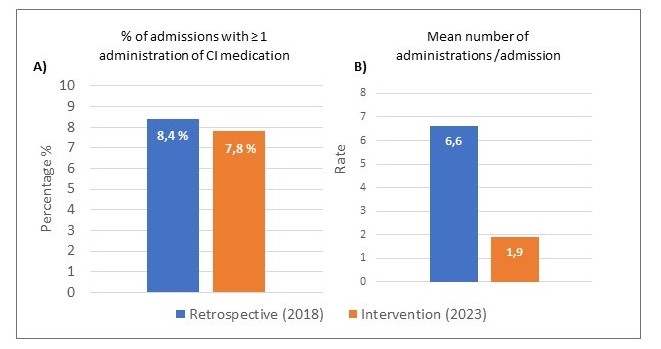
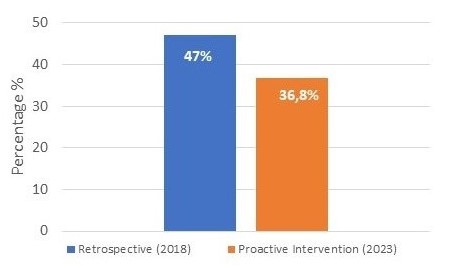
Results: There were 192 admissions from 149 unique primary parkinsonism patients. The team identified the need for bedside visits and/or interaction with the primary team in 122 admissions [table 1]. Fifteen out of 192 admissions (7.8%) received at least one administration of a contraindicated drug, similar to our retrospective cohort (8.4%). Of these admissions, the mean number of contraindicated drug administration per admission reduced from 6.6 in 2018 to 1.9 during the intervention [graph 1]. Outpatient levodopa dose timing information was available for 108 admissions (comprising 424 hospital days). Of these days, hospital dose timing intervals differed from home regimen intervals by greater than 30 minutes in 36.8%, compared to 47% in 2018 [graph 2].
Conclusion: The proactive intervention reduced both the number of contraindicated administrations per admission and the days with a deviation in levodopa timing interval. The impact of these improvements on clinical outcomes is under analysis.
Phone/ bedside interactions and support provided.
Administration of contraindicated medications.
Levodopa dose timing intervals.
References: [1] Yu JRT, Sonneborn C, Hogue O, Ghosh D, Brooks A, Liao J, Fernandez HH, Shaffer S, Sperling SA, Walter BL. Establishing a framework for quality of inpatient care for Parkinson’s disease: A study on inpatient medication administration. Parkinsonism Relat Disord. 2023 Aug;113:105491. doi: 10.1016/j.parkreldis.2023.105491. Epub 2023 Jul 7. PMID: 37495500.
To cite this abstract in AMA style:
C. Piccinin, J. Yu, A. Brooks, V. Stepanyants, P. Clark, S. Shaffer, B. Sokola, K. Lewin, C. Sonneborn, O. Hogue, S. Sperling, H. Fernandez, W. Walter. Preventing Medication Errors for Hospitalized People with Parkinson’s Disease – Results of Six Months of Proactive Intervention [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/preventing-medication-errors-for-hospitalized-people-with-parkinsons-disease-results-of-six-months-of-proactive-intervention/. Accessed July 14, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/preventing-medication-errors-for-hospitalized-people-with-parkinsons-disease-results-of-six-months-of-proactive-intervention/