Category: Parkinsonism, Atypical: MSA
Objective: To compare the Unified Multiple System Atrophy Rating Scale (UMSARS) part I-item 2 with an ear/nose/throat (ENT) expert physician assessment.
Background: Early and severe pharyngo-laryngeal signs, including dysphagia and stridor, are peculiar signs of Multiple system atrophy (MSA), possibly presenting a source of major disability and a predictor of poor outcome. MSA dysphagia is routinely assessed by the UMSARS part I-item 2.
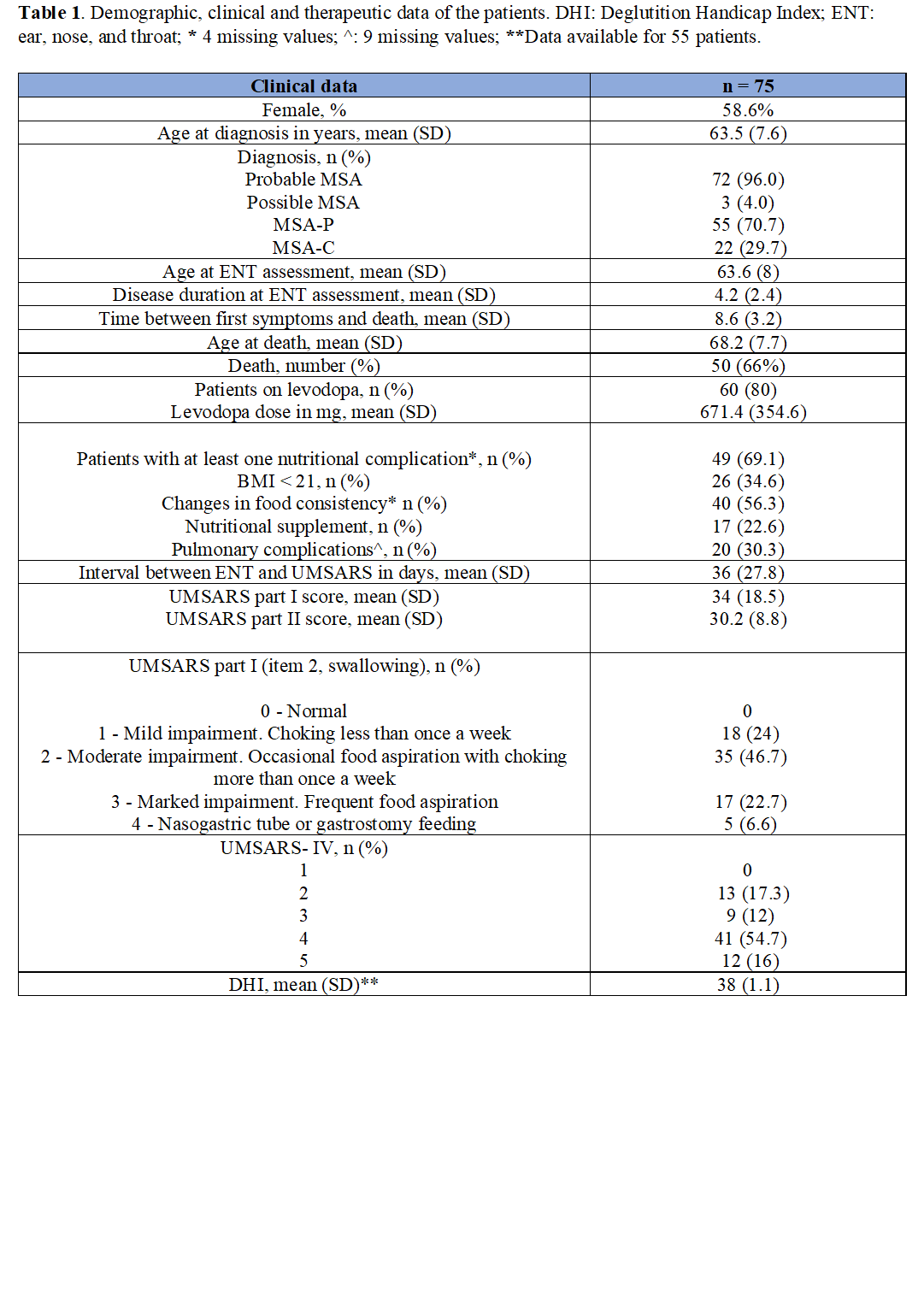
Method: We retrospectively analyzed the data of MSA patients who underwent an ENT assessment (nasofibroscopic and radioscopic exam) and an annual UMSARS assessment. Deglutition Handicap Index (DHI) and pulmonary/nutrition complications were collected.
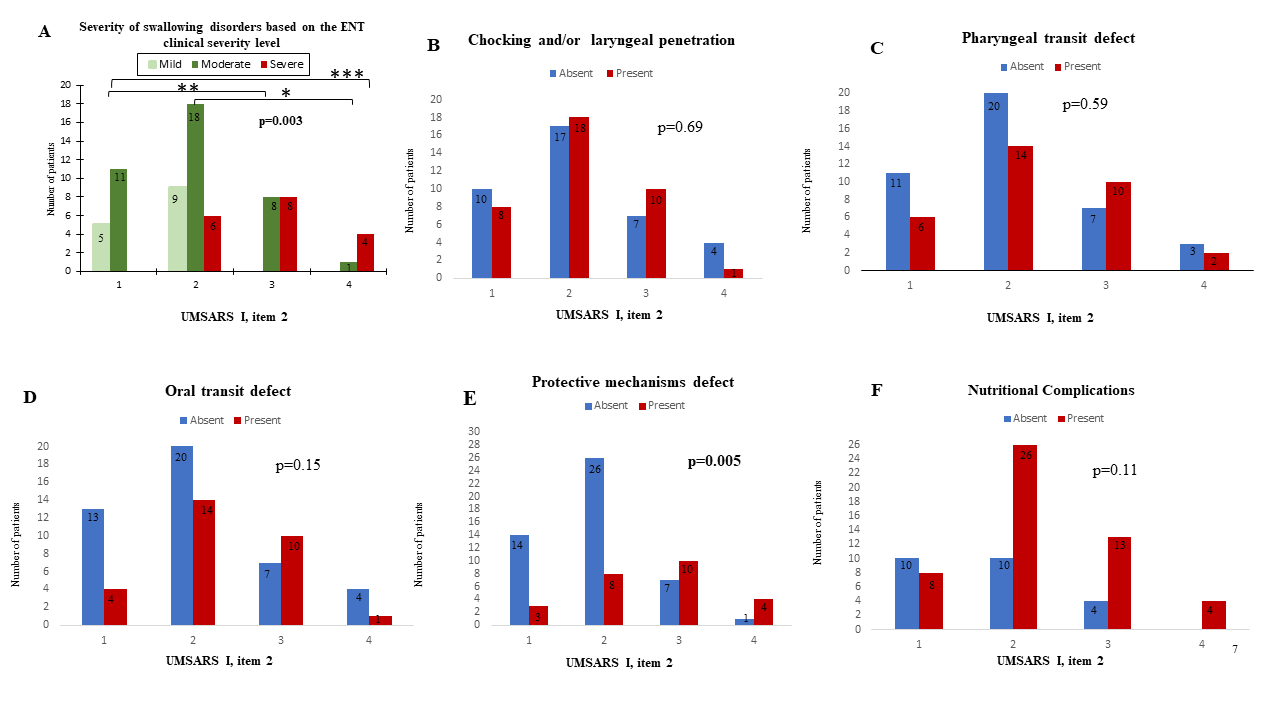
Results: Seventy-five MSA patients were included. Overall, patients had a mean (SD) age of 63.49 (7.56) years and a mean (SD) disease duration of 4.17 (2.35) years at the time of neurological/ENT assessment. According to the UMSARS “swallowing” item patients were classified as follows: 18 (24%) at level 1, 35 (46.6%) at level 2, 17 (22.6%) at level 3 and 5 (0.6%) level 4 with nasogastric tube or gastrostomy feeding (Table 1). The ENT assessment revealed more severe dysphagia compared to the UMSARS part I-item 2 score (p=0.003) (Figure 1). A higher proportion of patients with impaired protective mechanisms showed severe UMSARS-based dysphagia (p=0.005). Patients with choking and oral/pharyngeal transit defects and nutritional complications were equally distributed across UMSARS part I-item 2 scores. Worse UMSARS part I-item 2 scores had worse DHI scores.
Conclusion: The UMSARS-based assessment of dysphagia does not capture key aspects of pharyngo-laryngeal dysfunction reflecting swallowing efficiency. However, the early detection of these impairments by an ENT assessment may more efficiently allow the implementation of strategies to prevent malnutrition and aspiration pneumonia.
To cite this abstract in AMA style:
N. El Fassi, A. Pavy-Le-Traon, E. Mouchon, O. Rascol, W. Meissner, A. Foubert-Saumier, Y. Gallois, S. Tessier, F. Ory-Magne, V. Woizard, M. Fabbri. UMSARS versus laryngoscopy-based assessment of dysphagia [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/umsars-versus-laryngoscopy-based-assessment-of-dysphagia/. Accessed February 23, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/umsars-versus-laryngoscopy-based-assessment-of-dysphagia/