Category: Parkinsonism, Others
Objective: To differentiate Progressive Supranuclear Palsy (PSP) from Parkinson Disease (PD) using speech analysis.
Background: PD and PSP exhibit many clinical similarities including speech disorders early in the course of the disease but have substantially different prognosis [1], [2], [3]. Speech/voice analyses that are noninvasive, rapid, and simple to interpret represent a novel way to objectively and quantitatively differentiate between the two diagnoses [4], [5].
Method: Participants with probable PSP [6] or PD [7] were recruited. We recorded passage reading, counting, and sustained phonation on a custom tablet solution, and the software utilized automated speech recognition to transcribe the speech for pre-processing data. Pre-processed audio was then analyzed to extract phonatory, articulatory, prosody, and intelligibility features to distinguish PD from PSP. We also compared speech parameters to clinical features from the PSP Rating Scale, MDS-UPDRS and MoCA (e.g., dysarthria, dysphagia, bulbar scores, and cognition).
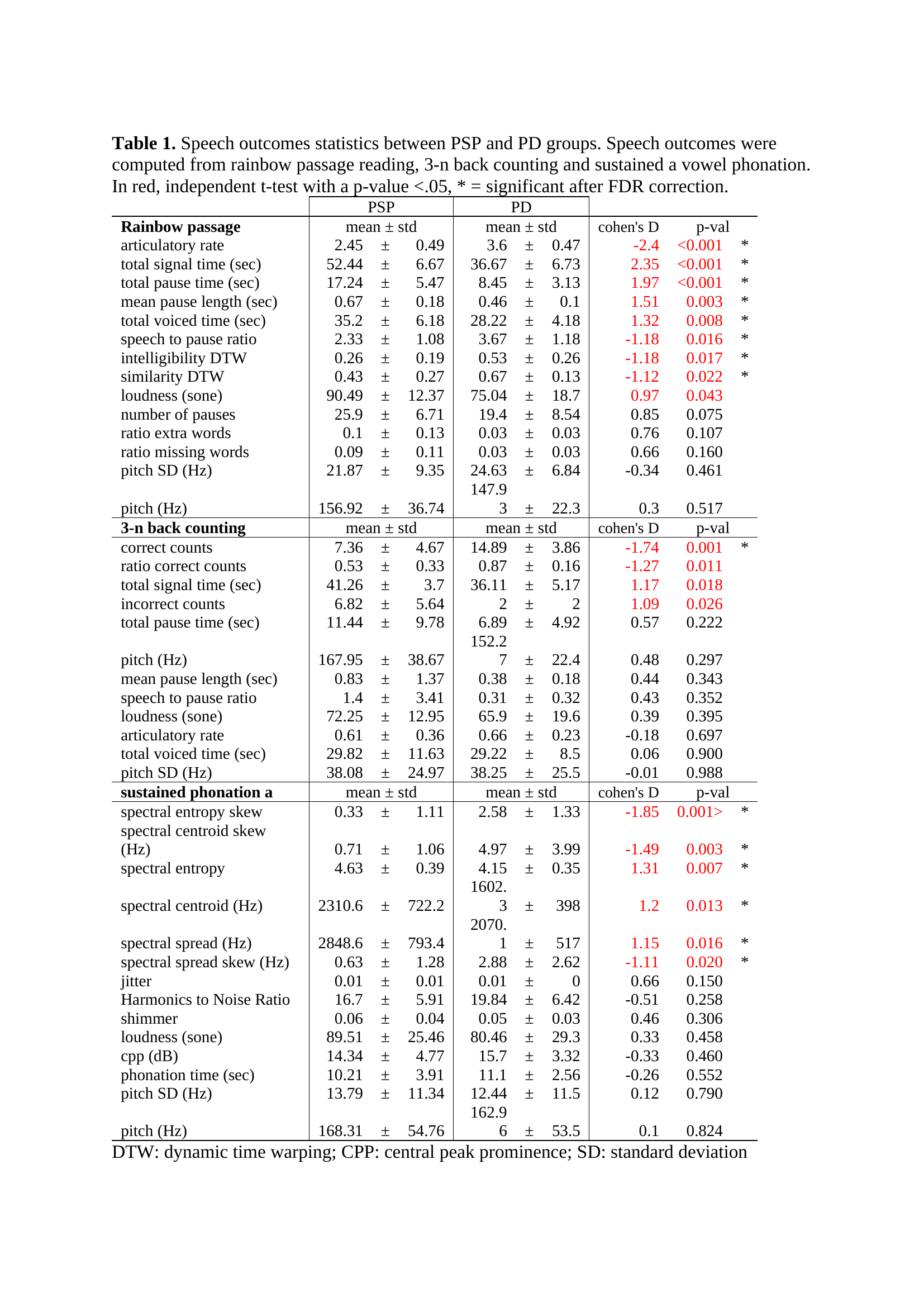
Results: Twenty-one participants were recruited (PSP (n=11), mean ± SD age =67.6 ±1.3, months since diagnosis=14 ± 3.5; PD (n=10), age 70.3 ±1.8, months since diagnosis=87.9 ±16.9). PSP had a slower articulation rate (2.45 ± 0.49 vs 3.60 ± 0.47 words/minute, Cohen’s d=-2.4, p<0.001), lower speech-to-pause ratio (2.33±1.08 vs 3.67±1.18, d =-1.18, p=0.016), intelligibility dynamic time warping (DTW, 0.26 ± 0.19 vs 0.53 ± 0.26, d=-1.18, p=0.017), and similarity DTW compared to PD (0.43 ± 0.27 vs 0.67 ± 0.13, d=-1.12, p=0.022). There was a longer total signal time (52.44±6.67 vs 36.67±6.73 sec, d=2.35, p<0.001) in PSP. PD had more accurate reverse number counts than PSP (14.89 ± 3.86 vs 7.36 ± 4.67, d=-1.74, p=0.001). PSP also demonstrated higher uncertainty (4.63 ± 0.39 vs 4.15 ± 0.35, d=1.31, p=0.007) and spectral spread (2848.6±793.40 vs 2070.1±517.00 Hz, d=1.15, p=0.016) for sustained ‘a’ phonation. Correct reverse number counts were positively correlated with total MoCA scores (r=0.703, p= 0.016).
Conclusion: Our study demonstrates the feasibility of differentiating PSP from PD using a digital health technology platform. Developing quantitative, observer-independent, real-time, clinical measures for noninvasive monitoring of people with PD and PSP is an important step toward improving clinical trials and early diagnosis.
References: References
[1] C. H. Adler et al., “Low clinical diagnostic accuracy of early vs advanced Parkinson disease: Clinicopathologic study,” Neurology, vol. 83, no. 5, pp. 406–412, Jul. 2014, doi: 10.1212/WNL.0000000000000641.
[2] I. Litvan et al., “Accuracy of clinical criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome),” Neurology, vol. 46, no. 4, pp. 922–930, 1996.
[3] J. Rusz et al., “Speech disorders reflect differing pathophysiology in Parkinson’s disease, progressive supranuclear palsy and multiple system atrophy,” Journal of neurology, vol. 262, pp. 992–1001, 2015.
[4] B. Das, K. Daoudi, J. Klempir, and J. Rusz, “Towards disease-specific speech markers for differential diagnosis in parkinsonism,” in ICASSP 2019-2019 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), 2019, pp. 5846–5850.
[5] J. Rusz et al., “Acoustic assessment of voice and speech disorders in Parkinson’s disease through quick vocal test,” Movement Disorders, vol. 26, no. 10, pp. 1951–1952, 2011.
[6] G. U. Hoglinger et al., “Clinical Diagnosis of Progressive Supranuclear Palsy: The Movement Disorder Society Criteria,” Mov Disord, vol. 32, no. 6, pp. 853–864, Jun. 2017, doi: 10.1002/mds.26987.
[7] R. B. Postuma et al., “MDS clinical diagnostic criteria for Parkinson’s disease,” Movement disorders, vol. 30, no. 12, pp. 1591–1601, 2015.
To cite this abstract in AMA style:
K. Kang, A. Nunes, M. Sharma, A. Hall, R. Mishra, J. Casado, R. Cole, G. Barchard, A. Vaziri, A. Wills, A. Pantelyat. Utilizing Speech Analysis to Differentiate Progressive Supranuclear Palsy from Parkinson Disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/utilizing-speech-analysis-to-differentiate-progressive-supranuclear-palsy-from-parkinson-disease/. Accessed February 18, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/utilizing-speech-analysis-to-differentiate-progressive-supranuclear-palsy-from-parkinson-disease/