Category: Parkinson's Disease: Cognitive functions
Objective: Assess performance on computerized illusions across PD patients with (PD_Hal) and without (PD_NonHal) history of visual hallucinations and explore underlying cortical substrates.
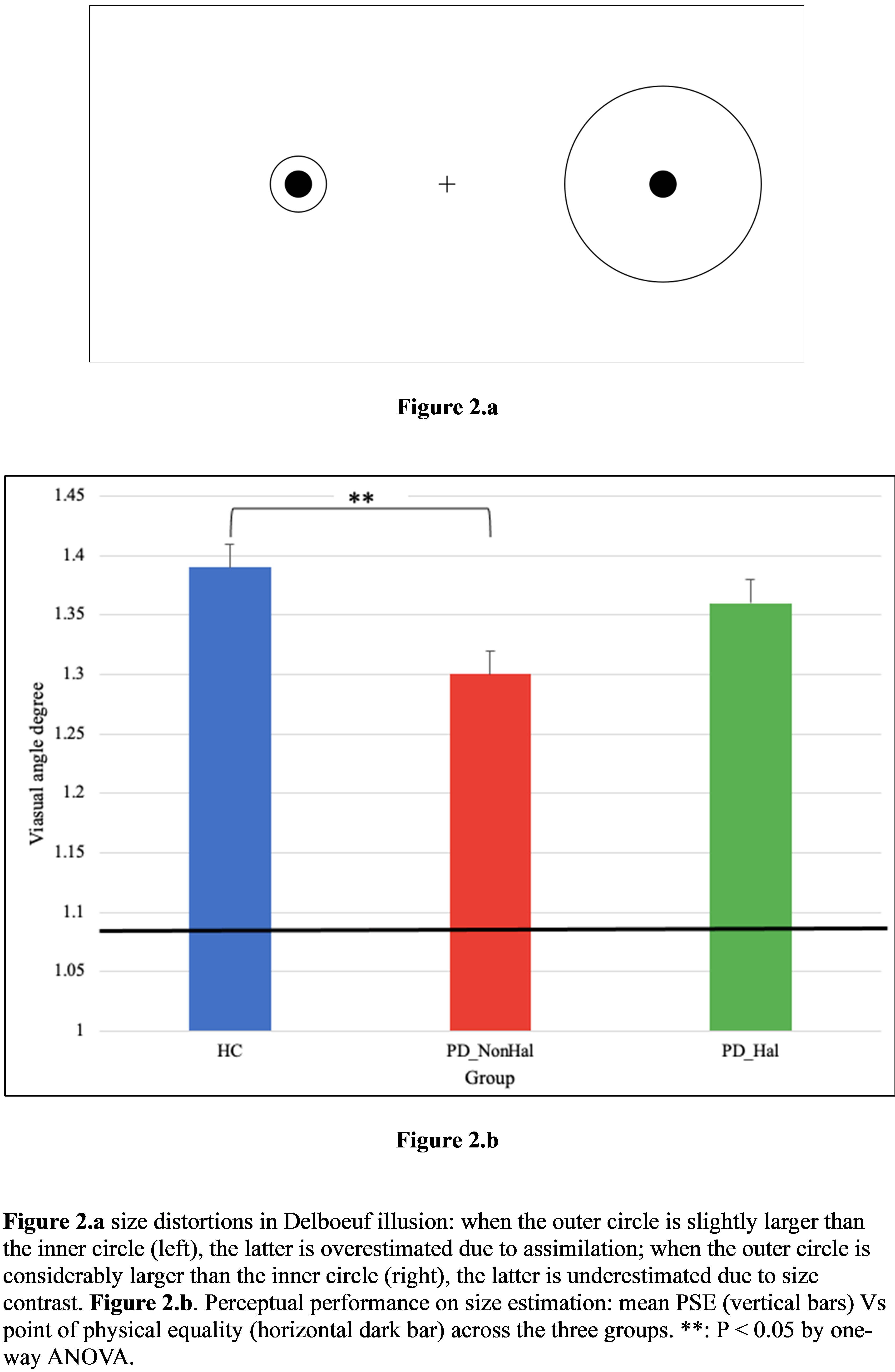
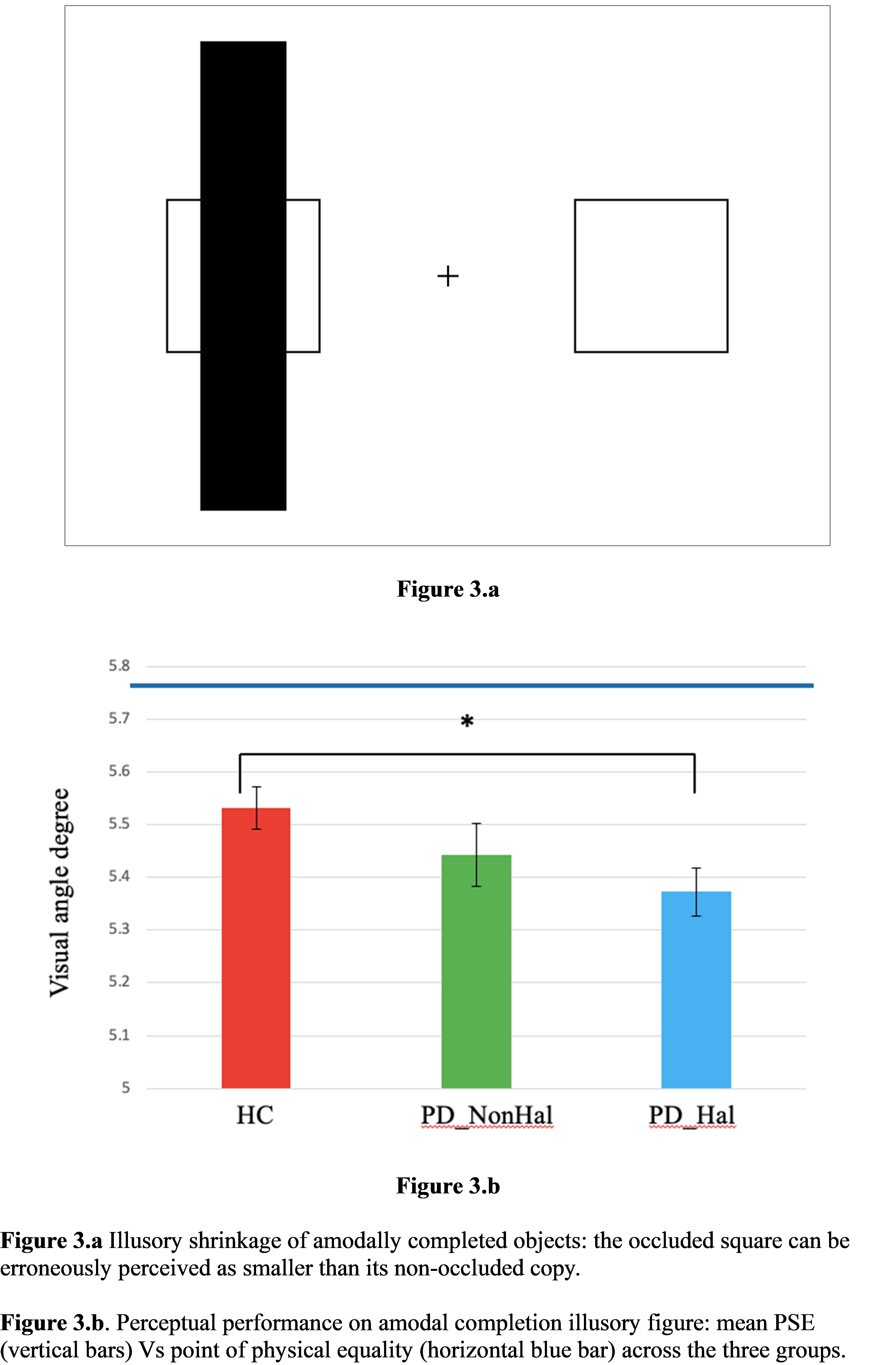
Background: In healthy individuals, illusions are induced by parametric manipulations of visual stimuli. In the Delboeuf illusion (DB), two identical circles (targets) are surrounded by bigger circles (inducers). If targets and inducers are close, targets are assimilated with inducers and overestimated. In the shrinkage of amodal completion (AC), partially occluded objects are perceived as smaller than their non-occluded copies.
Method: Eligibility included MoCA ≥24, intact acuity and no ocular disease. Hallucinatory status was based on the UMPDHQ. When attending the DB and AC, subjects reported which target and square was bigger, respectively. Subjective points of equality were determined with a staircase method. MDS-UPDRS and PDQ39 assessed clinical severity and quality of life (QoL). Cortical substrates were explored on 18FDG PET. One-way ANOVA was run with PSE as dependent variable. Clinical variables and Z scores were compared by t-test (significance at P <0.05).
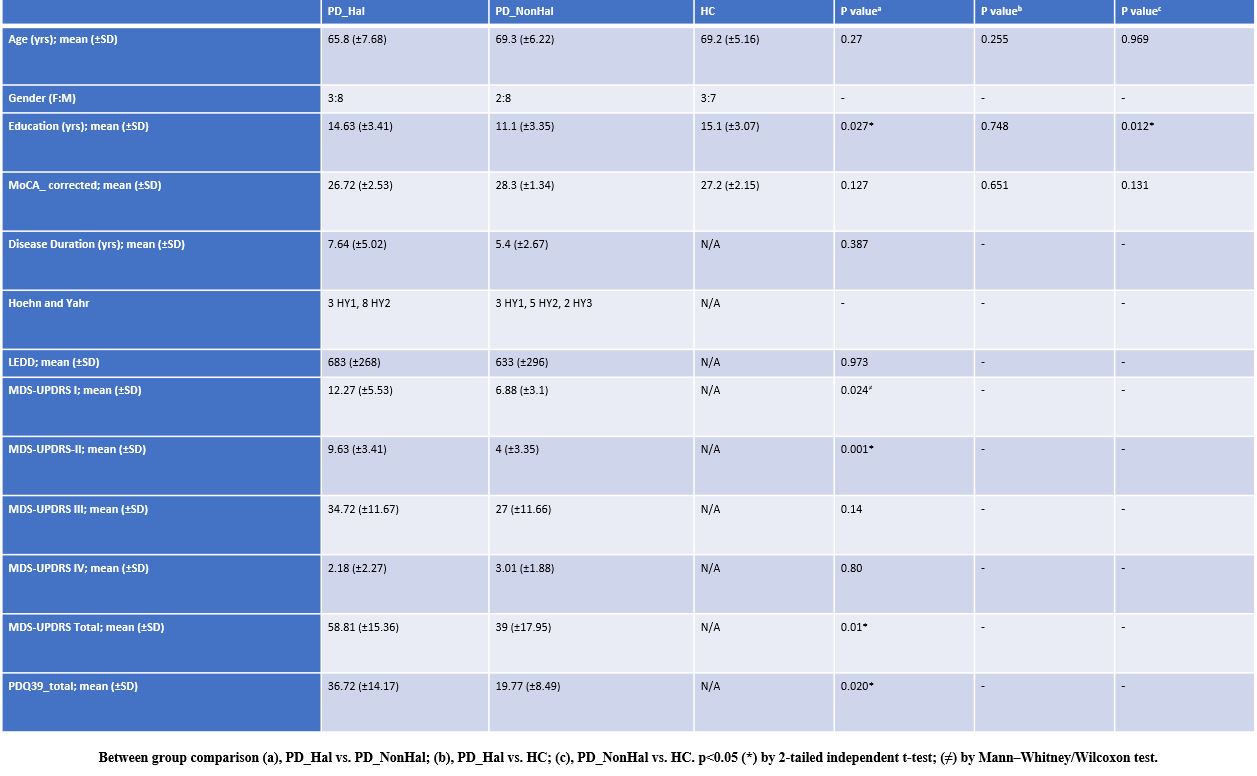
Results: Ten PD_Hal, 11 PD_NonHal and 10 healthy controls (HC) were recruited. Disease duration, staging, treatment, and motor severity were comparable across PD groups, with poorer QoL in PD_Hal (Figure 1). On DB, PD_NonHal performed significantly better than HC. Performance of PD_Hal did not differ from HC (Figure 2). Performance on AC was better in HC followed by PD_NonHal, and PD_Hal (Figure 3). Diffuse hypometabolism was found in PD. Hypoactivation was significantly lower in the medial prefrontal cortex of PD_Hal. Posterior hypometabolism was more pronounced in PD_Hal.
Conclusion: PD_NonHal were more resistant to the DB than HC. The DB implies the co-activation of extrastriate (spatial computation) and frontal cortices (set-shifting). Impaired attentional modulation and overreliance on local analysis may have reduced the assimilation distortion in these patients. PD_Hal were more vulnerable to the AC. Impaired figure/background and overlapping figures segregation may explain this finding. Both require intact occipital-prefrontal connectivity. PET findings suggest abnormal top-down modulation in PD_Hal, with lower prefrontal hypoactivation, of likely compensatory nature. Abnormal attention, spatial scaling and grouping are key drivers of hallucinations in PD.
Demographics and Clinical Features
Delboeuf Illusion
Illusory Shrinkage of Amodal Completion
References: Weil RS, Reeves S. Hallucinations in Parkinson’s disease: new insights into mechanisms and treatments. Adv Clin Neurosci Rehabil.;19(4); (2020).
Thomas GEC, Zeidman P, Sultana T, Zarkali A, Razi A, Weil RS. Changes in both top-down and bottom-up effective connectivity drive visual hallucinations in Parkinson’s disease. Brain Commun. 4;5(1); (2022).
To cite this abstract in AMA style:
A. Cucca, M. Catalan, M. Liccari, TMI. Lombardo, V. Cenacchi, S. Rangan, CV. Manara, S. Mingolo, M. Murgia, T. Agostini, P. Manganotti. Abnormal Top-down Perceptual Modulation Drives Visual Hallucinations in Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/abnormal-top-down-perceptual-modulation-drives-visual-hallucinations-in-parkinsons-disease/. Accessed July 9, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/abnormal-top-down-perceptual-modulation-drives-visual-hallucinations-in-parkinsons-disease/