Category: Allied Healthcare Professionals
Objective: To analyze differences in baseline characteristics of patients at a new diverse, academic Parkinson’s Disease (PD) interdisciplinary clinic (IDC).
Background: The University of Miami (UM) recently opened a PD IDC where patients are evaluated by neurology, physical and occupational therapy, nutrition, speech and language pathology, social work, and neuropsychology providers during one session. The patient population seen in its first year has been previously described [1], however with the inclusion of more patients in its second year, comparative analyses of differences in baseline measures of disease severity can now be performed.
Method: We performed a retrospective chart review of all patients evaluated in the UM PD IDC from January 1, 2022 – September 1, 2023. Statistical analysis included Chi-square, 2-sample 2-tailed independent t-tests, and correlations. Statistical significance was set at p=0.05.
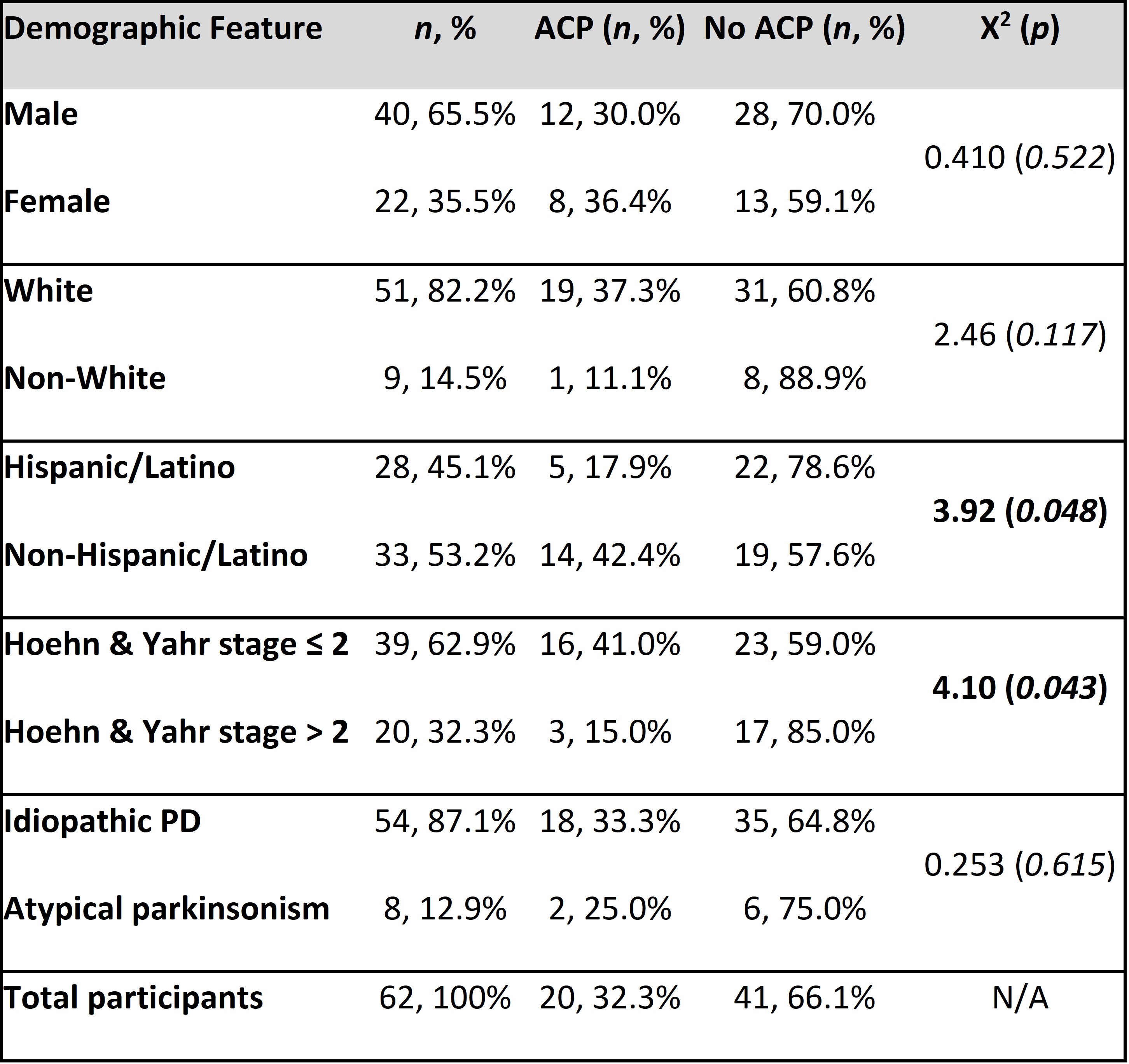
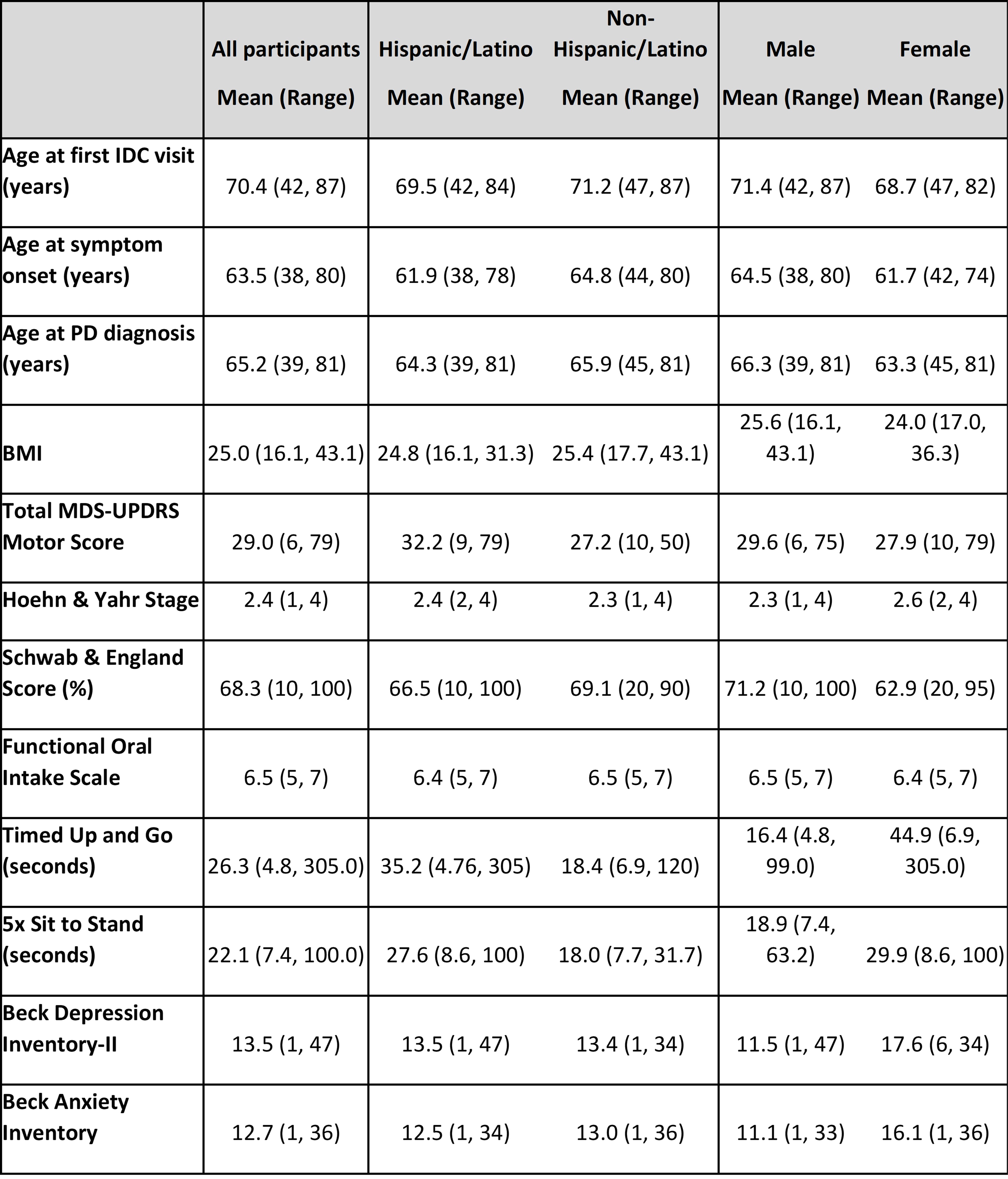
Results: Sixty-two patients were seen at the IDC in its first year, of which 35.5% were female, 82.2% were White, and 45.2% identified as Hispanic. Hispanic and female patients performed significantly worse on the 5x sit to stand test than non-Hispanic and male patients (27.6 vs. 18.0 sec, p=0.04 and 29.9 vs. 18.9 sec, p=0.02, respectively). Females had a significantly higher mean HY stage at the time of referral (2.6 vs. 2.3, p=0.045); Hispanics similarly had a higher mean HY stage but this did not reach statistical significance.
Conclusion: There is a large knowledge gap surrounding the impact of race and ethnicity on PD. [2,3] Our IDC, with its robust Hispanic population, has the potential to illuminate further ethnic and racial differences as patients are followed longitudinally. Among patients seen in the clinic, Hispanic and female patients performed worse on the 5x sit to stand test, and females had significantly higher HY stage at the time of referral. We suspect that this is due to a trend towards female and Hispanic patients presenting to the IDC later in their disease course. The reason for this may include patient factors, referral bias, or other disparities in access to healthcare. Further directions for this research include longitudinal follow-up of our patients, as well as further study to determine which patients may benefit most from the IDC, to guide referrals and reduce disparities in access.
Demographics, presence of advanced care planning.
Baseline characteristics.
References: 1. Armengol V, Sarno M, Feldman M, et al. A baseline study for the first year of a diverse Parkinson’s Disease interdisciplinary clinic [abstract]. Mov Disord. 2023;38 (suppl 1).
2. Sauerbier A, Aris A, Lim EW, Bhattacharya K, Ray Chaudhuri K. Impact of ethnicity on the natural history of Parkinson disease. Med J Aust. 2018;208(9):410-414.
3. Ben-Joseph A, Marshall CR, Lees AJ, Noyce AJ. Ethnic Variation in the Manifestation of Parkinson’s Disease: A Narrative Review. J Parkinsons Dis. 2020;10(1):31-45.
To cite this abstract in AMA style:
V. Armengol, M. Feldman, M. Sarno, S. Marmol, A. Alfonso, G. Dumenigo, M. Garcia-Casals, S. Munzesheimer, A. Otto, TW. Siu, D. Yacinthe, D. Shpiner. An Analysis of Baseline Measures from a Diverse Parkinson’s Disease Interdisciplinary Clinic [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/an-analysis-of-baseline-measures-from-a-diverse-parkinsons-disease-interdisciplinary-clinic/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/an-analysis-of-baseline-measures-from-a-diverse-parkinsons-disease-interdisciplinary-clinic/