Category: Parkinson's Disease: Pathophysiology
Objective: To determine if neuropsychiatric and axial motor symptoms at baseline would be predictive of freezing of gait (FoG) at 5-year follow up in participants with Parkinson’s Disease (PD) from the Parkinson’s Progression Markers Initiative (PPMI) study.
Background: Retrospective cohorts have found that neuropsychiatric (depressive symptoms and cognitive dysfunction [1,2]) and some axial motor symptoms (dysarthria [3], but not dysphagia [4]) have been associated with FoG. However, it has yet to be seen if neuropsychiatric or axial motor symptoms may serve as predictors of FoG.
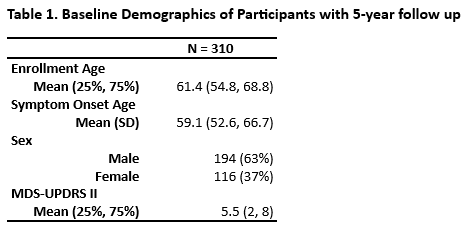
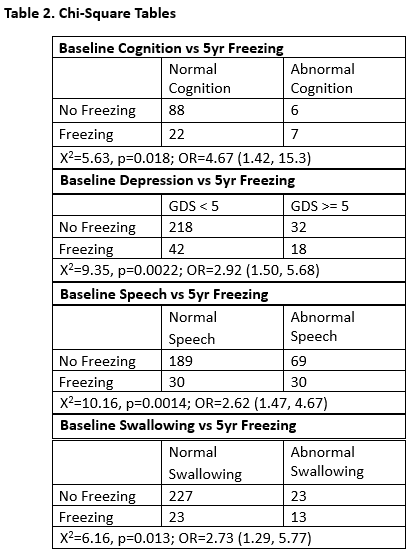
Method: Clinical data from PPMI, a multicenter prospective study of Parkinson’s disease followed from early onset, was analyzed to see if neuropsychiatric or axial motor symptoms reported at baseline in participants who did not have FoG at that time was associated with a higher likelihood of having FoG at 5-year follow up assessment than those who did not have these symptoms at baseline. Neuropsychiatric symptoms included cognitive impairments and depression. Cognition was determined as normal or abnormal (mild cognitive impairment or dementia) based on the clinician’s response to the Cognitive Categorization questionnaire. Depression was identified as having a Geriatric Depression Scale (GDS) score >= 5. Axial motor symptoms included speech and swallowing difficulties. Speech and Swallowing was categorized based on subjects’ responses to MDS-UPDRS items 2.1 and 2.3. Scores of 0 were considered as normal, and >0 as abnormal. Chi-squared tests were used to assess for demographic differences between the cohort at baseline and at 5-year follow up.
Results: Amongst those who did not have FoG at baseline, all measures were associated with an increased likelihood of FoG at 5-year follow-up (Cognition: OR=4.67(1.42, 15.3), p=0.018; Depression: OR=2.92(1.50, 5.68), p=0.0022; Speech: OR=2.62(1.47, 4.67), p=0.0014; Swallowing: OR=2.73(1.29, 5.77), p=0.013) (Fig. 2).
Conclusion: Cognitive impairments, depression, dysarthria, and dysphagia may be useful prognostic markers for FoG. It has yet to be seen if physical therapy intervention before FoG onset can delay the time to FoG or first fall.
Table 1. Baseline demographics of Participants
Table 2. Chi-Square Tables
References: 1. Taximaimaiti R, Wang XP. Comparing the Clinical and Neuropsychological Characteristics of Parkinson’s Disease With and Without Freezing of Gait. Front Neurosci. 2021;15:660340. Published 2021 Apr 27. doi:10.3389/fnins.2021.660340
2. Nieuwboer A, Giladi N. Characterizing freezing of gait in Parkinson’s disease: models of an episodic phenomenon. Mov Disord. 2013;28(11):1509-1519. doi:10.1002/mds.25683
3. Mekyska J, Galaz Z, Kiska T, et al. Quantitative Analysis of Relationship Between Hypokinetic Dysarthria and the Freezing of Gait in Parkinson’s Disease. Cognit Comput. 2018;10(6):1006-1018. doi:10.1007/s12559-018-9575-8
4. C. Kobylecki, I. Shiderova, E. Michou. Relationship between dysphagia severity and gait disturbance in Parkinson’s disease [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/relationship-between-dysphagia-severity-and-gait-disturbance-in-parkinsons-disease/. Accessed March 8, 2024.
To cite this abstract in AMA style:
J. Li, R. Rajmohan, J. Ruiz Tejeda, N. Phielipp. Assessing the Predictive Accuracy of Baseline Neuropsychiatric and Axial Motor Features for Freezing of Gait in Parkinson’s Disease at 5-year Follow up: The PPMI Cohort [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/assessing-the-predictive-accuracy-of-baseline-neuropsychiatric-and-axial-motor-features-for-freezing-of-gait-in-parkinsons-disease-at-5-year-follow-up-the-ppmi-cohort/. Accessed July 3, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/assessing-the-predictive-accuracy-of-baseline-neuropsychiatric-and-axial-motor-features-for-freezing-of-gait-in-parkinsons-disease-at-5-year-follow-up-the-ppmi-cohort/