Category: Parkinson's Disease: Cognitive functions
Objective: This study aims to explore the BP profile in both PD-MCI and PDD
Background: Blood pressure (BP) abnormality is often correlated with cognitive impairment. However, there was no sufficient data on BP profile in Parkinson’s disease (PD) patients with cognitive impairment, whether mild cognitive impairment (PD-MCI) or dementia (PDD)
Method: All PD patients who were on their scheduled visit to Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia, consecutively from October to December 2023, in this cross-sectional study. Basic demographic and clinical data were obtained. We assessed the cognitive function using Indonesian version of Scales for Outcomes in Parkinson’s disease-Cognition (SCOPA-Cog INA)
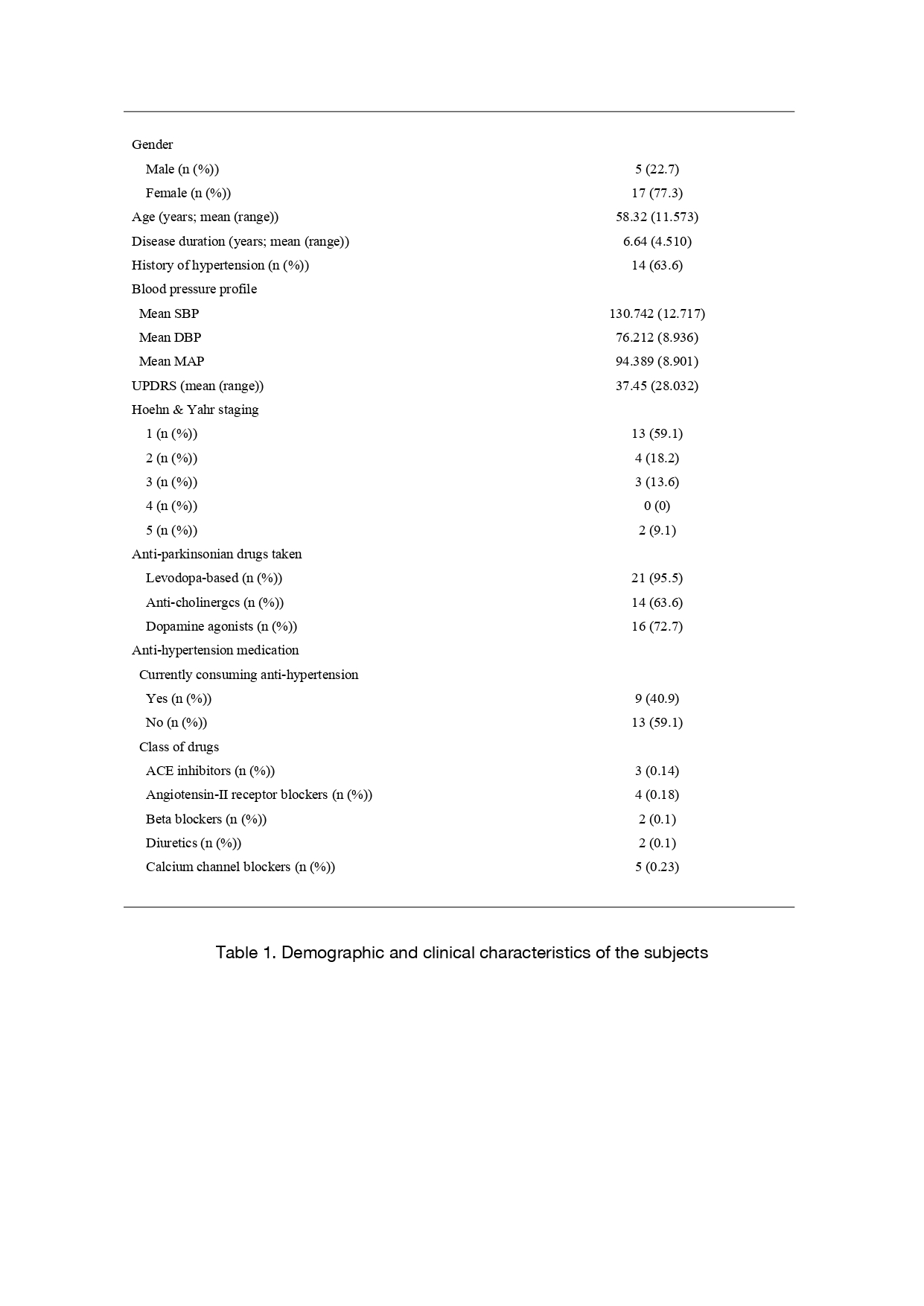
Results: From 22 PD subjects, 77.3% were female, with mean age of 58.32±11.57 years old, mean disease duration of 6.64±4.51 years, and 63.6% had a history of hypertension (HT). The mean systolic blood pressure (SBP) is 130.74±12.72, while mean diastolic blood pressure (DBP) and mean arterial pressure (MAP) was 76.21±8.94 and 94.39±8.9. Mean score of SCOPA-Cog INA was 21.86±7.611. Most common antihypertension medication (AHM) was calcium channel blockers (0.23%), followed by angiotensin-II receptor blockers (0.18%) and ACE inhibitors (0.14%)
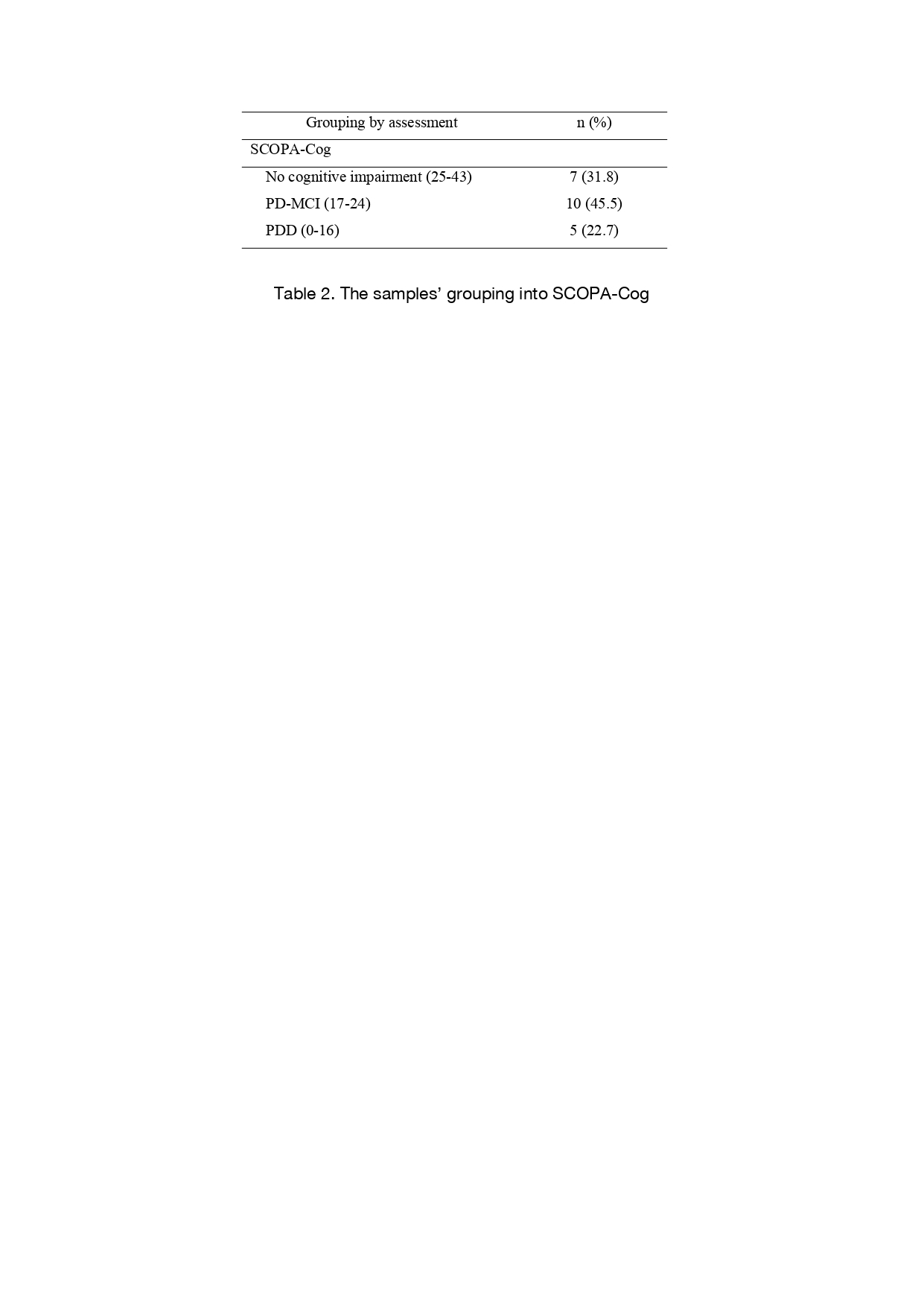
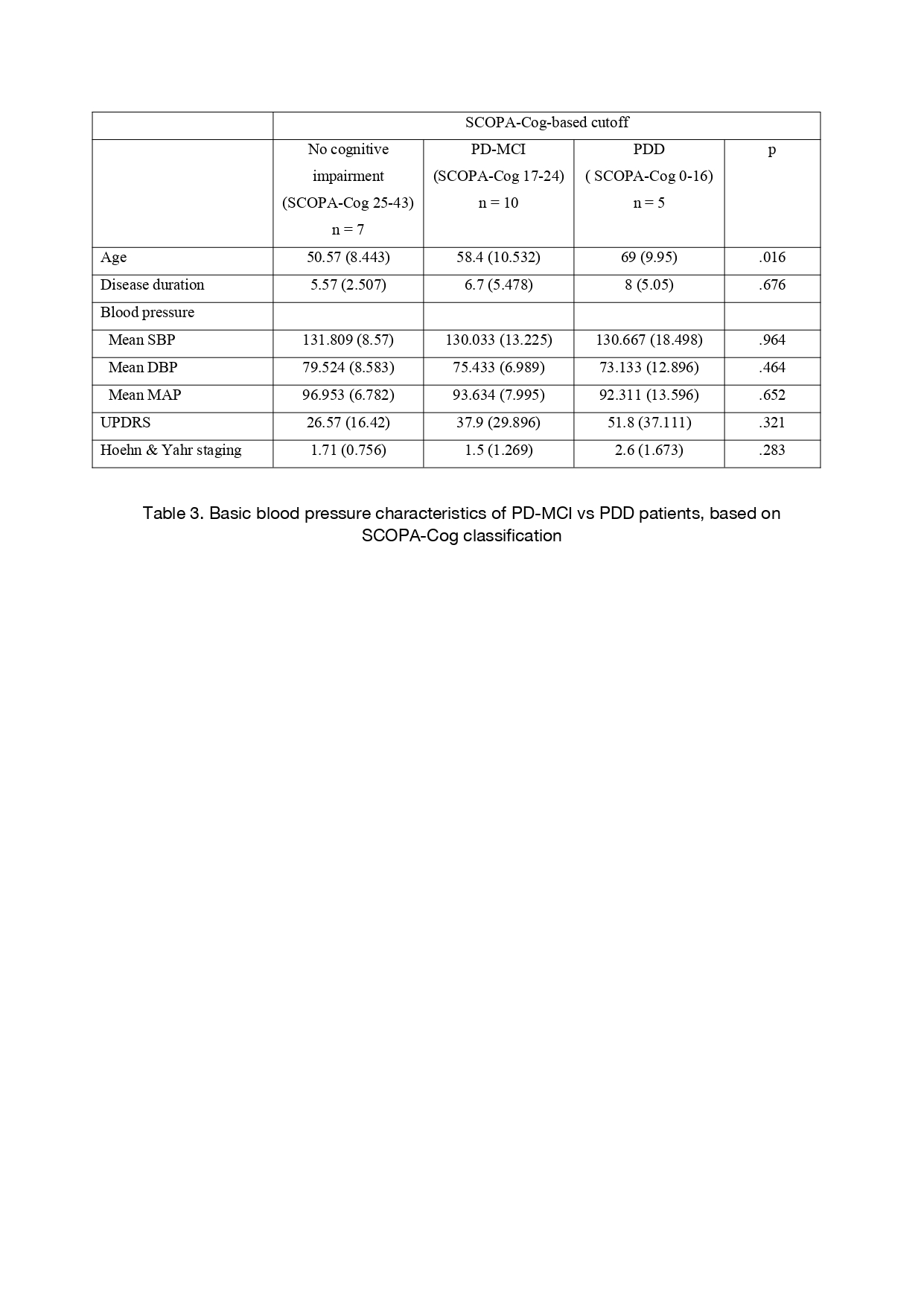
Using SCOPA-Cog INA, we classified the subjects into three groups: no cognitive impairment, PD-MCI, and PDD. PDD subjects were found to had the oldest age (69±9.95; p<0.05). There was no significant difference (p>0.05) on the mean SBP, DBP, and MAP between the groups, although subjects with no cognitive impairment had the highest mean SBP, DBP, and MAP. PDD subjects had greater disease progression (UPDRS 51.8±37.111; Hoehn-Yahr 2.6±1.673), although it was not significant (p>0.05)
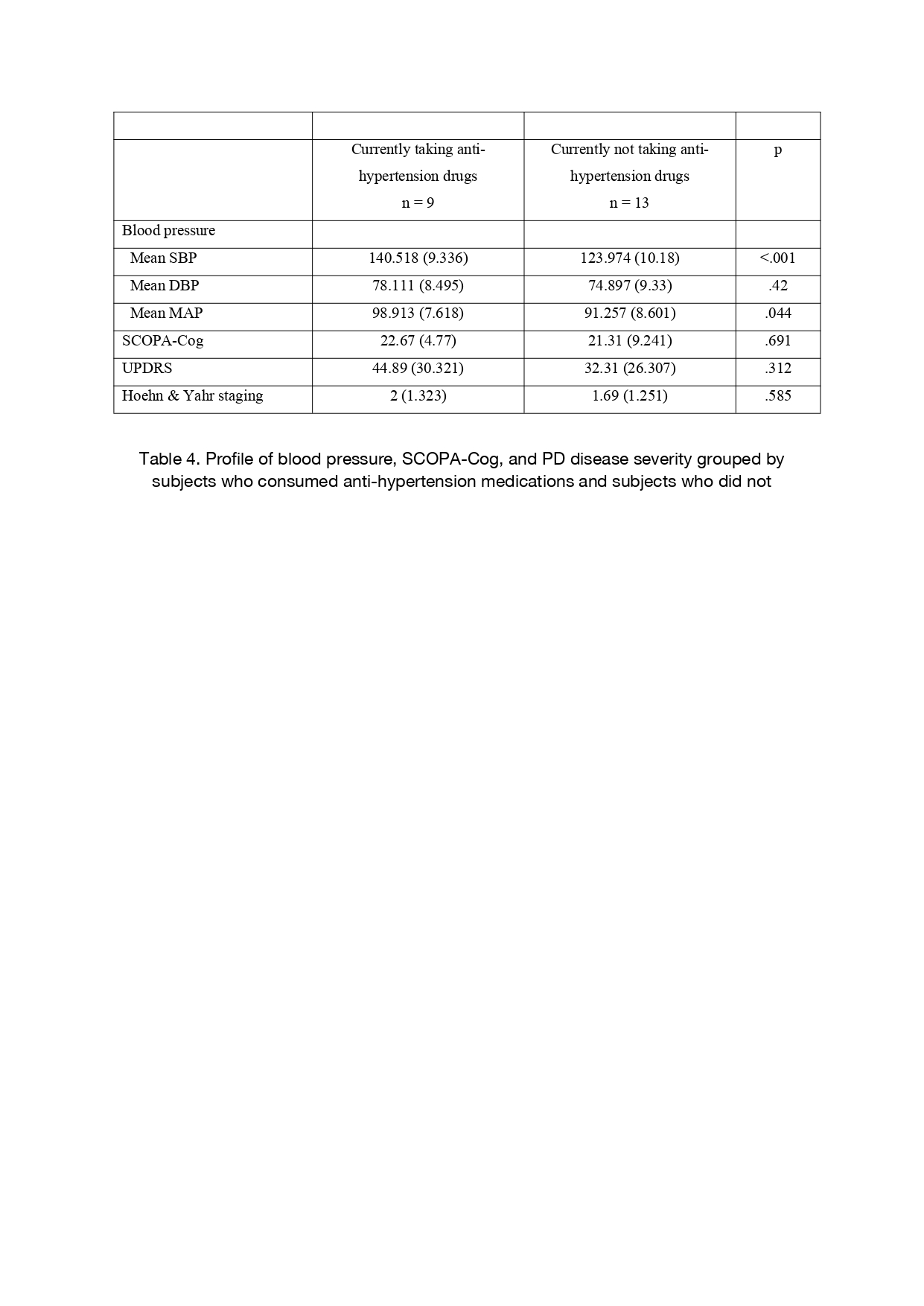
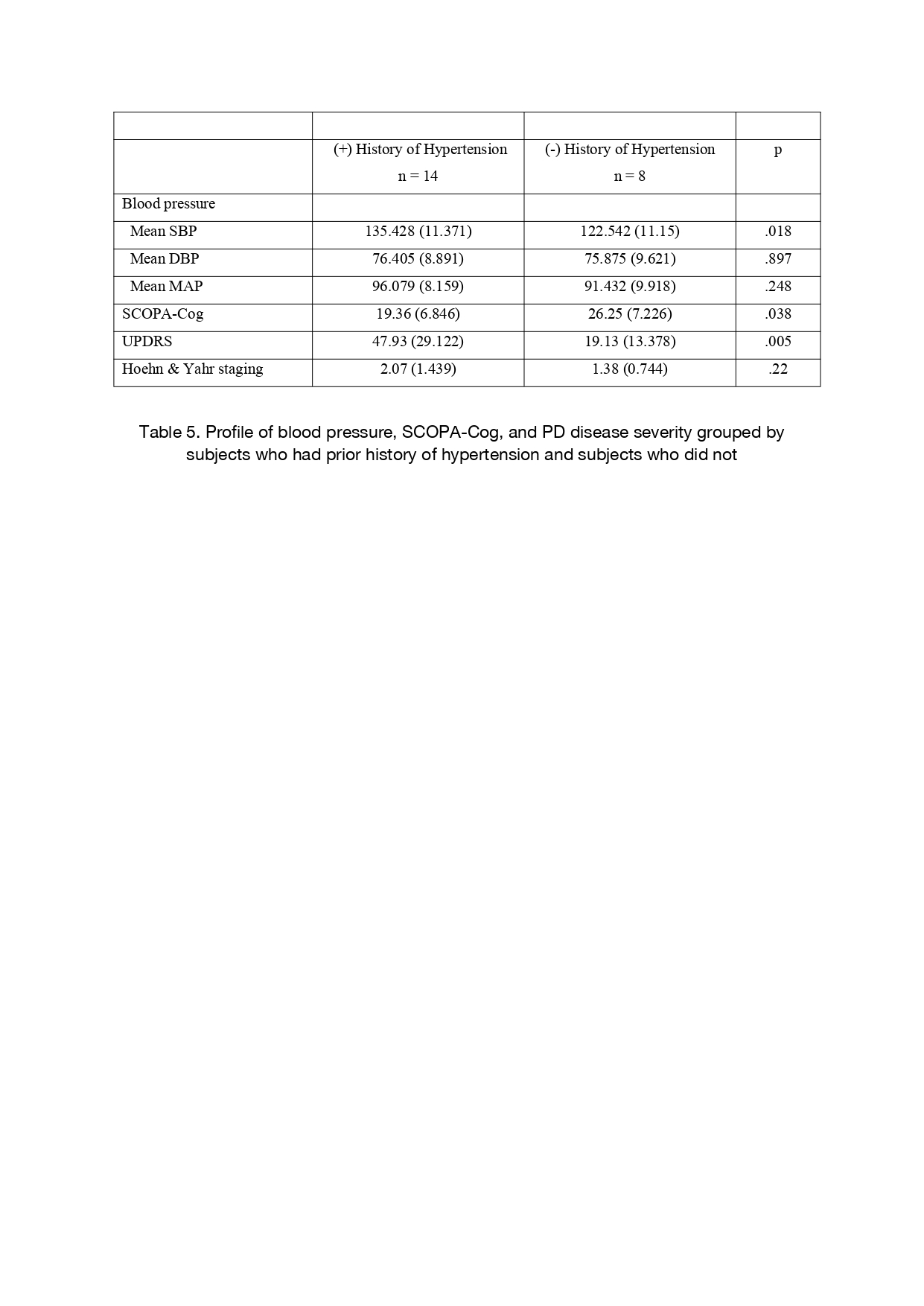
Mean SBP and MAP was significantly (p<0.001; p<0.05) higher in subjects who took AHM (140.518±9.336 vs 129.74±10.18; 98.913±7.618 vs 91.257±8.601). Mean SBP was also found significantly (p<0.05) higher in subjects who had prior history of HT (135.428±11.37 vs 122.542±11.15). Subjects with prior history of HT also showed worse SCOPA-Cog INA (19.36±6.846 vs 26.25±7.226; p<0.05) and UPDRS scores (47.93±29.122 vs 19.13±13.378; p<0.05)
Conclusion: Vascular changes might be one of the underlying cause of cognitive changes in PD subjects. Further research is necessary to explore the relation between BP indices and cognitive function in PD subjects
Table 1
Table 2
Table 3
Table 4
Table 5
References: 1. V. Isella, C. Mapelli, N. Morielli, Siri C, D. De Gaspari, G. Pezzoli, et al. Diagnosis of possible Mild Cognitive Impairment in Parkinson’s disease: Validity of the SCOPA-Cog. Parkinsonism & Related Disorders. 2013 Dec 1;19(12):1160–3.
2. Balal M, Demirkiran M, Paydas S. Central Aortic Pressure and Arterial Stiffness in Parkinson’s Disease: A Comparative Study. Fereshtehnejad SM, editor. Parkinson’s Disease. 2022 Jul 12;2022:1–8.
3. Shindo K, Morishima Y, Suwa Y, Fukao T, Kurita T, Satake A, et al. Age‐related changes in blood pressure and heart rates of patients with Parkinson’s disease. The Journal of Clinical Hypertension. 2020 Nov 17;23(1):175–8.
4. Riley DE, Espay AJ. Cognitive fluctuations in Parkinson’s disease dementia: blood pressure lability as an underlying mechanism. Journal of Clinical Movement Disorders. 2018 Feb 13;5(1).
To cite this abstract in AMA style:
A. Al Jody, A. Tiksnadi, D. Tunjungsari. Blood Pressure Profile of PD-MCI and PDD in Parkinson’s Disease Patients at Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/blood-pressure-profile-of-pd-mci-and-pdd-in-parkinsons-disease-patients-at-dr-cipto-mangunkusumo-hospital-jakarta-indonesia/. Accessed July 1, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/blood-pressure-profile-of-pd-mci-and-pdd-in-parkinsons-disease-patients-at-dr-cipto-mangunkusumo-hospital-jakarta-indonesia/