Objective: To present a cohort report on the physical decline and impact on activities of daily life (ADL) of prolonged bedrest for Atypical Parkinsonism’s syndrome (APS) patients. The study aims to suggest Physiotherapy (PT) limitations for motor degenerative conditions.
Background: A 2007 study showed that experimentally induced bedrest in healthy young males for 5 weeks leads to decreased physical and structural capabilities. A loss of muscular density, bone loss and an inability to recover pre-bedrest activity levels within 4 weeks of rehabilitation [1]. APS conditions are characterised by physical decline and patients admitted to hospitals are at risk of deconditioning at greater rates than at home.
Method: Using online patient clinic reports, 3 patients from each APS group, Multiple System Atrophy (MSA), Cortical Basal Syndrome (CBS) and Progressive Supranuclear Palsy (PSP), were assessed. 1 patient of all groups underwent hospitalisation for reasons not due to APS and experienced prolonged bed rest. Themes of ADL and mobility were assessed and compared to before-bedrest levels.
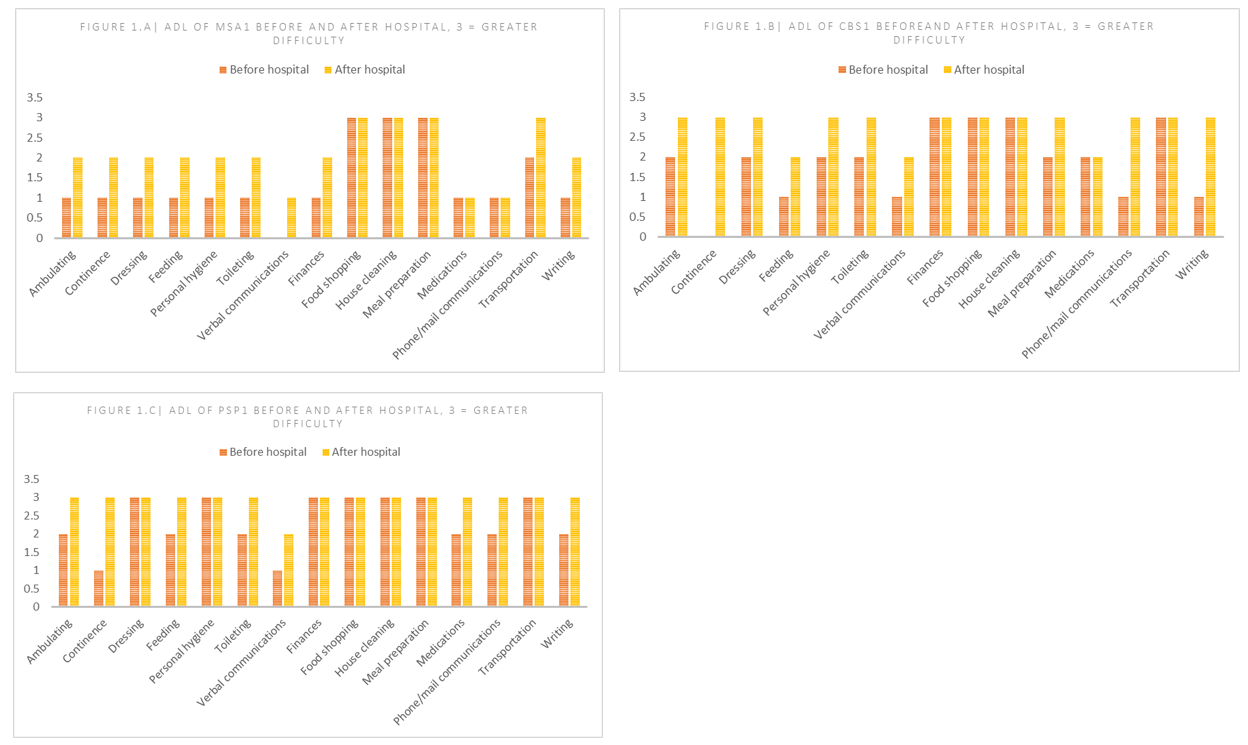
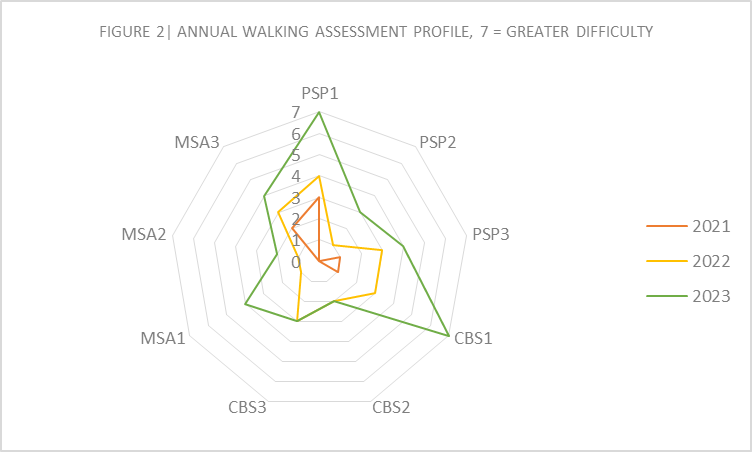
Results: ADL’s subscale compares patient’s ability to perform tasks before and after hospitalisation (figure 1). It shows an increase in dependence on carers for basic and instrumental activities by 22.2%, 31.1% and 20% for MSA, CBS and PSP hospitalised patients, respectively. A mobility decline is reflected in the increase in walking aids from 2021-2023 for all patients (figure 2). Based on mean comparisons, hospitalised patients’ difficulty in walking was 100% greater in 2023, after hospitalisation, and only 22% greater in 2022, the year before admission, compared to non-hospitalised patients.
Conclusion: All APS patients exhibited physical deconditioning and greater dependence on carers for ADL showing PT could not recover pre-onset levels of mobility but aids a slower rate of progression in a patient’s mobility decline. A link between bedrest and deconditioning of APS patients is observed as 2 of the hospitalised patients were bedbound and remained immobile despite PT rehabilitation. Observations showed that physical abilities were lost (sitting up or transferring) without consistent engagement in PT or carer-aided exercises. Data suggests that the approach to APS patient care in hospitals needs to accommodate increased deconditioning upon admission.
Figure 1
Figure 2
References: [1] Berg, H. E., Eiken, O., Miklavcic, L., & Mekjavic, I. B. (2007). Hip, thigh and calf muscle atrophy and bone loss after 5-week bedrest inactivity. European journal of applied physiology, 99(3), 283–289. https://doi.org/10.1007/s00421-006-0346-y
To cite this abstract in AMA style:
A. Mimpriss, J. Donnelly, L. Massey, B. Ghosh. Cohort study and Review on Physiotherapy in the Rehabilitation and Pro-longed Bed Rest of Atypical Parkinsonism’s Syndrome Patients [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/cohort-study-and-review-on-physiotherapy-in-the-rehabilitation-and-pro-longed-bed-rest-of-atypical-parkinsonisms-syndrome-patients/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/cohort-study-and-review-on-physiotherapy-in-the-rehabilitation-and-pro-longed-bed-rest-of-atypical-parkinsonisms-syndrome-patients/