Category: Parkinsonism, Atypical: PSP, CBD
Objective: We aimed to develop a clinical scale that distinguishes between Multiple System Atrophy (MSA) and 4-repeat tauopathies (4RT: CBD, PSP) using a standardized neurological examination based on signs commonly observed in atypical parkinsonian syndromes.
Background: Currently, there is a lack of bedside assessments to aid in the differential diagnosis of these conditions, despite the frequent overlap in low probability criteria for 4RT and MSA in the early stages of the disease.
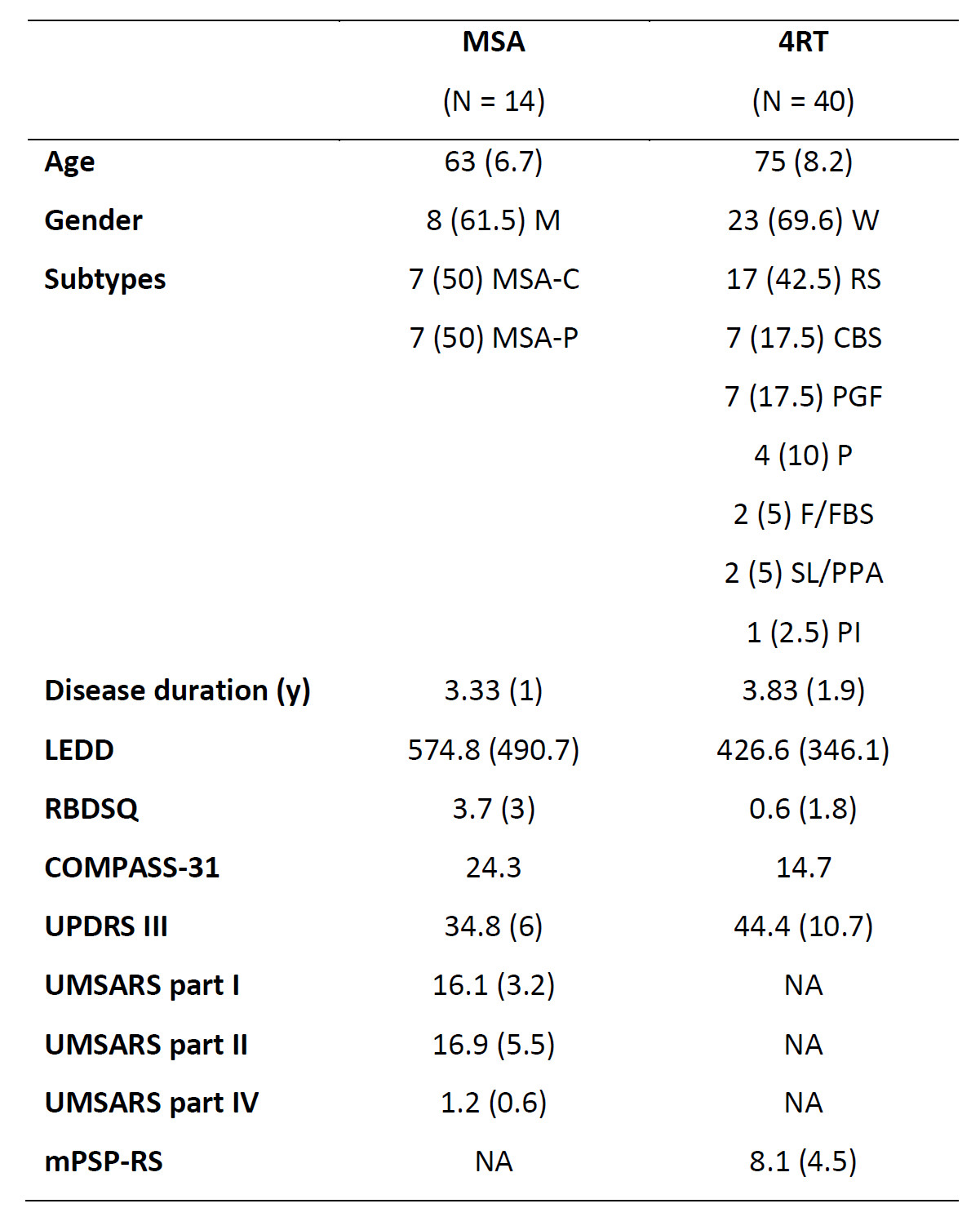
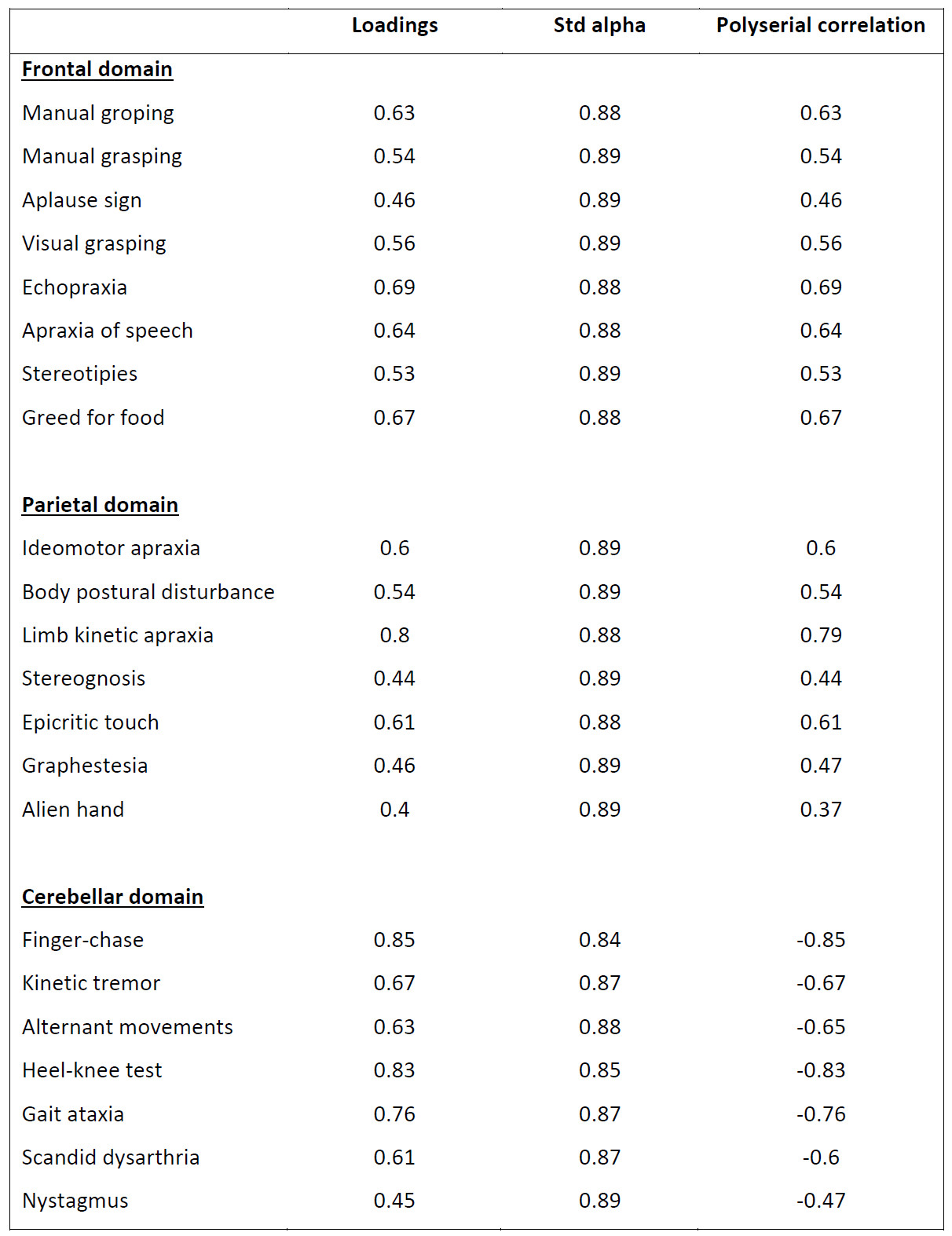
Method: 54 patients with <4 years from symptom onset were recruited at Hospital Sant Pau, from the Atypical Parkinsonian Disorders Clinic (table 1). A gold standard for the diagnosis of MSA and 4RT was established through assessment by two independent neurologists, and additional tests such as MRPI 2.0 index, FDG-PET, MIBG, and polysomnography were performed in uncertain cases when overlap of diagnostic criteria. The initial scale assessed the degree of impairment in four domains: frontal, parietal, oculomotor and cerebellar. Scale refinement included polyserial analysis, exploratory factorial analysis, and reliability analysis. Confirmatory factorial analysis was conducted for the final scale. Validation included a machine learning approach and structural MRI markers in a subgroup of patients.
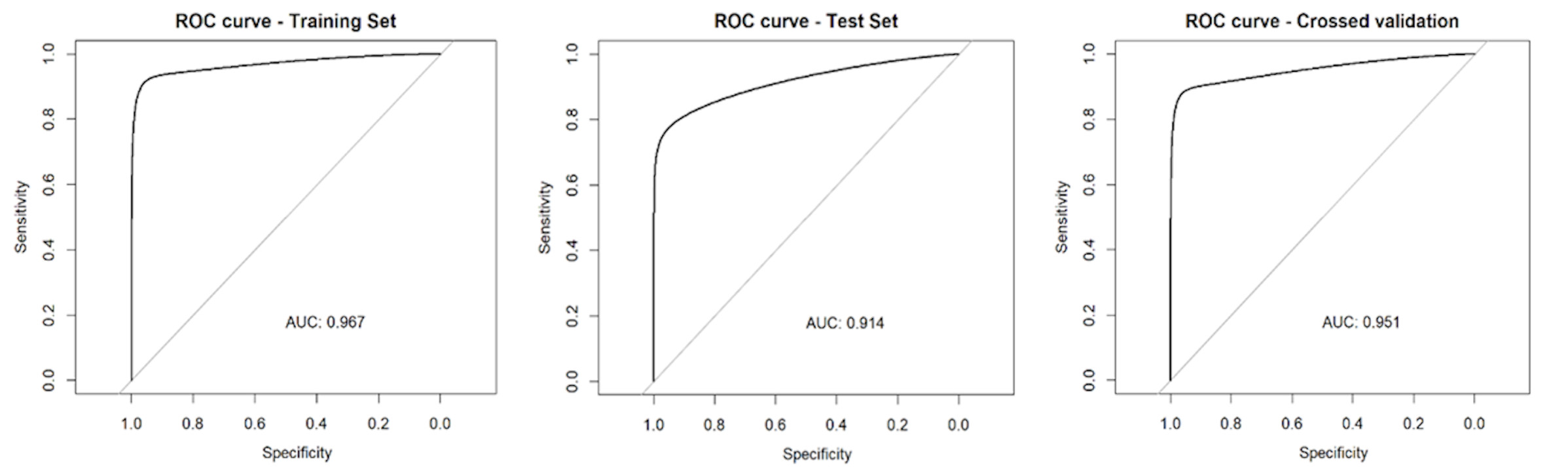
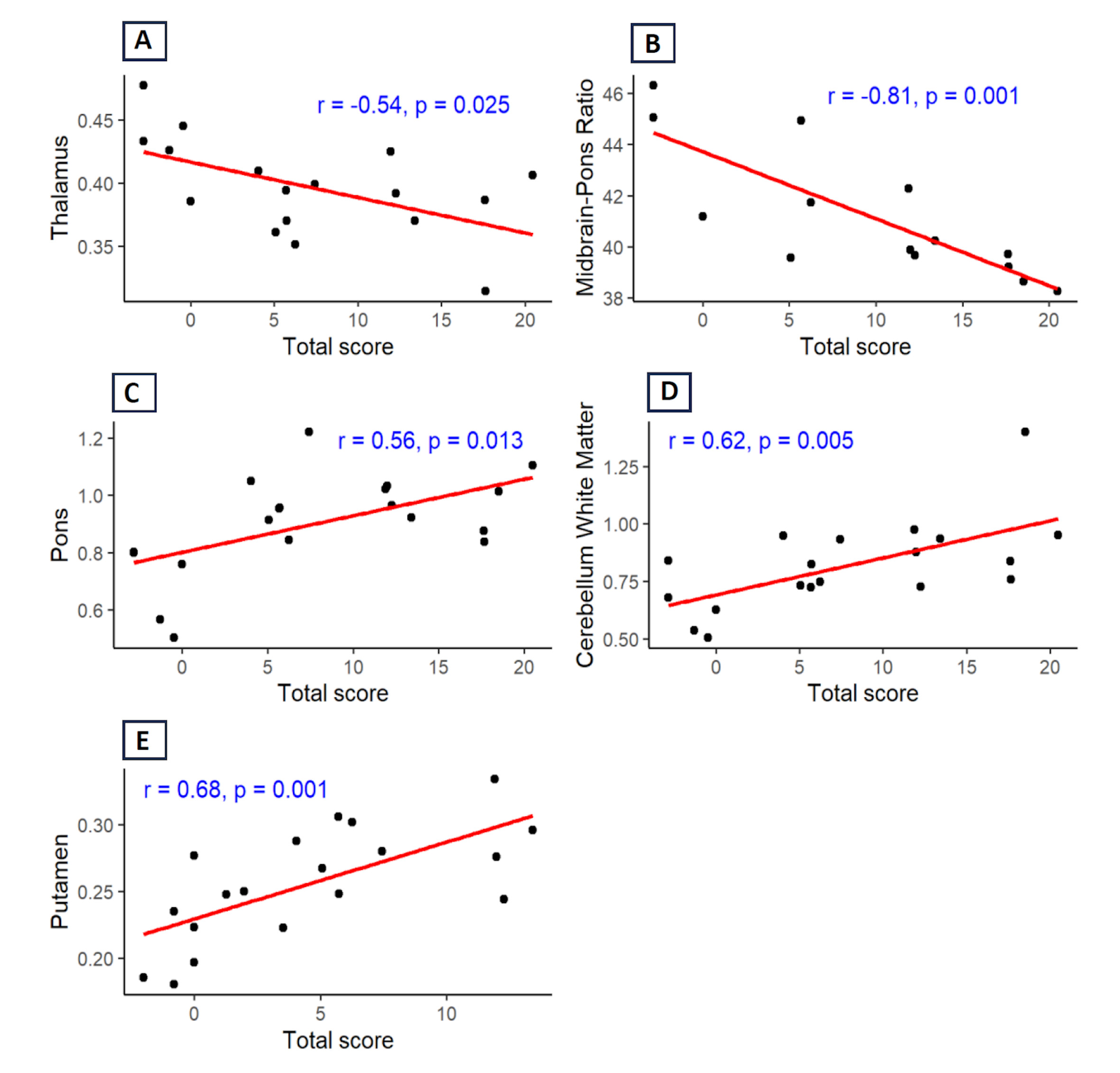
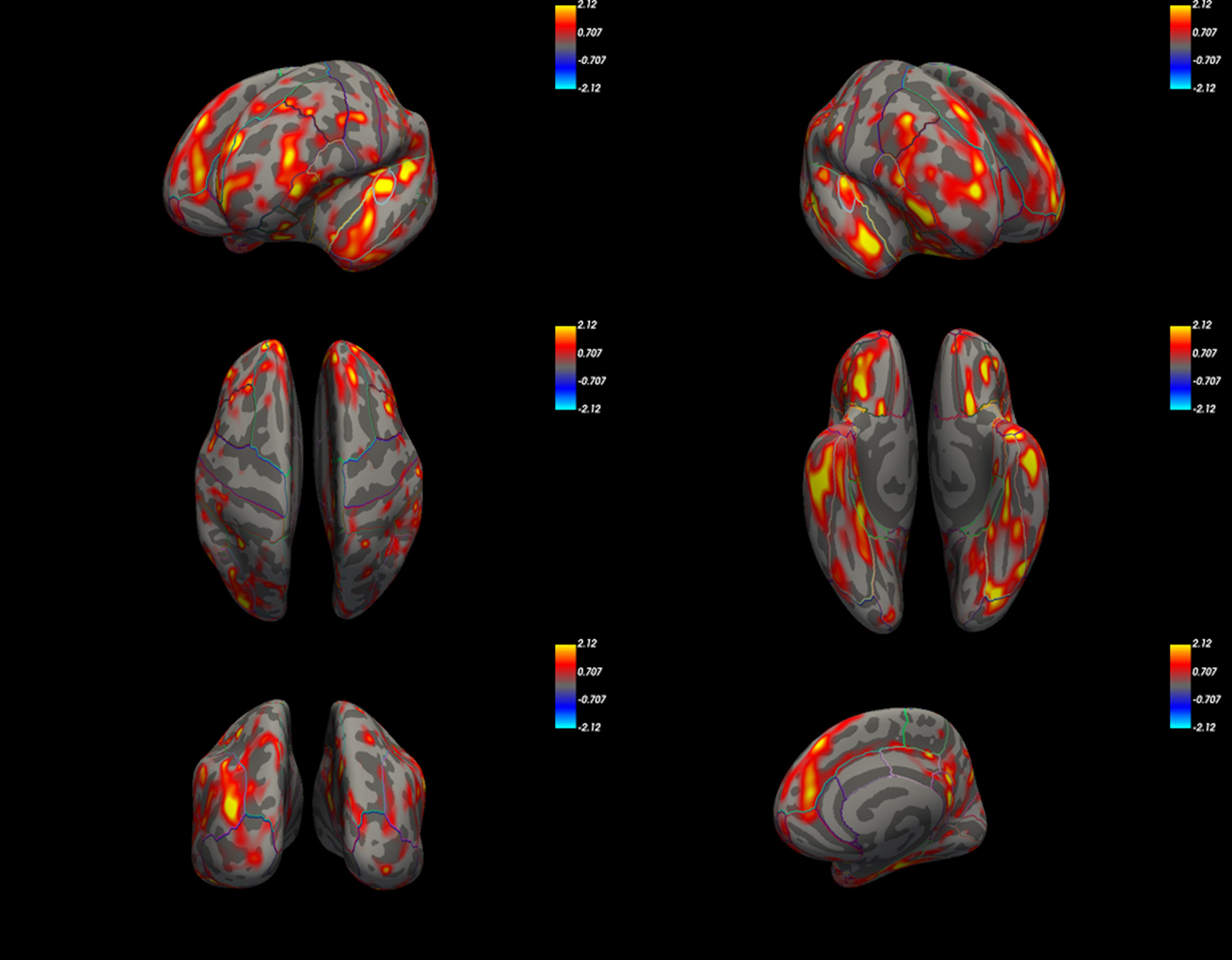
Results: During scale refinement, four items were eliminated from the frontal domain, three from the parietal domain, and the oculomotor domain was removed. The scale structure analysis and item reduction showed significant improvement, with favorable outcomes in reliability analysis (table 2). Higher scores in frontal and parietal domains were associated with increased likelihood of 4RT, while lower scores correlated with higher probability of MSA. Machine learning analysis using the LASSO regularized logistic regression model exhibited robust performance. Cross-validation confirmed consistent model performance with average sensitivity of 85.71% and specificity of 90%. ROC curves are shown on figure 1. Neuroimaging analysis revealed significant correlations between subcortical volumes and the scale’s total score (figure 2). A cutoff score of 2 emerged as a potentially optimal threshold for distinguishing between MSA and 4RT based on cortical thickness analysis (figure 3).
Conclusion: This newly developed quantitative bedside scale has the potential to enhance diagnostic accuracy in distinguishing MSA from 4RT.
Table 1
Table 2
Figure 1
Figure 2
Figure 3
To cite this abstract in AMA style:
I. Ruiz Barrio, A. Horta Barba, A. Puig Davi, I. Aracil Bolaños, A. Quattrone, S. Martinez Horta, J. Kulisevksy, J. Pagonabarraga. Development and Validation of a Clinical Scale for Distinguishing Multiple System Atrophy from 4-Repeat Tauopathies [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/development-and-validation-of-a-clinical-scale-for-distinguishing-multiple-system-atrophy-from-4-repeat-tauopathies/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/development-and-validation-of-a-clinical-scale-for-distinguishing-multiple-system-atrophy-from-4-repeat-tauopathies/