Session Information
Date: Sunday, October 7, 2018
Session Title: Phenomenology and Clinical Assessment Of Movement Disorders
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: To investigate whether self-report, clinical, and physical therapy (PT) assessments differ in identifying freezing of gait (FOG) in Parkinson’s disease (PD).
Background: Most studies rely on self-report assessments when identifying FOG. The Movement Disorders Society- Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) is a commonly used, reliable scale to assess multiple aspects of PD, and includes an item on Part III for the clinician to rate freezing. However, brief observations in the clinic as well as the patient’s self-assessment may not be sufficient to identify an episodic phenomenon. Freezing of gait may occur more frequently at home than in the clinical setting.
Methods: 15 PD patients enrolled in an ongoing study (Center for Neurodegeneration and Translational Neuroscience) were assessed for FOG. FOG questionnaire Item 3 was used for self-report. MDS-UPDRS Part III Item 11 was used for clinical assessment. The FOG assessment score, which includes several conditions that commonly trigger FOG, was used as a PT assessment. MDS-UPDRS and PT assessments were done in the OFF state (without levodopa). The statistical agreement between measures was analyzed by generalized kappa.
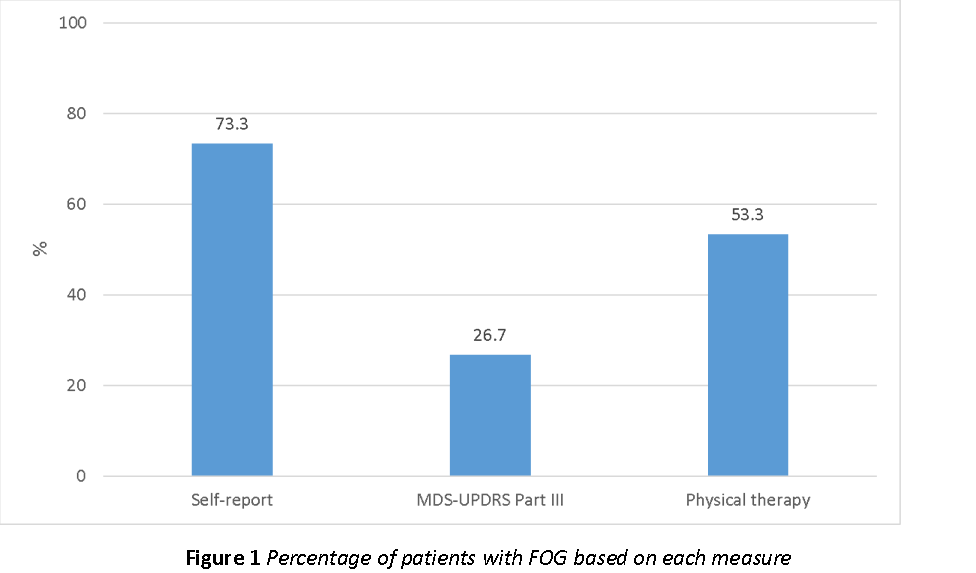
Results: 11 patients self-reported FOG, 4 patients had FOG according to MDS-UPDRS, and 8 patients had FOG according to PT [figure 1]. All subjects who had FOG according to MDS-UPDRS also had freezing on PT and self-report. All subjects with freezing during PT had self-reported freezing. The kappa value for the agreement between the measures was 0.377.
Conclusions: There is a discrepancy between all recorded measures of FOG, even in a small sample size. Patients tend to over-report the presence of FOG, whereas longer evaluation periods and inclusion of FOG triggering conditions increase the chance of FOG occurrence compared to brief clinical assessment. Future studies may consider inclusion of a PT assessment to identify FOG in PD patients to obtain more reliable results. Wearable monitors and remote technology may better objectively quantify PD-FOG.
To cite this abstract in AMA style:
B. Bluett, E. Bayram, J. Longhurst, S. Banks, Z. Mari, I. Litvan. Discrepancies in assessments of freezing of gait: Self-report, clinical, and physical therapy assessments [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/discrepancies-in-assessments-of-freezing-of-gait-self-report-clinical-and-physical-therapy-assessments/. Accessed February 13, 2026.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/discrepancies-in-assessments-of-freezing-of-gait-self-report-clinical-and-physical-therapy-assessments/