Objective: To investigate the influence of age-associated vestibulopathy (presbyvestibulopathy, PVP) on dynamic gait and balance in Parkinson’s disease (PD) patients and elderly controls. We hypothesized that despite the presence of PVP in both groups, postural impairments might be more severe in PD.
Background: PVP manifests in neurologically intact aging adults and those with PD, an age-associated neurodegenerative disorder. While the vestibular system naturally undergoes frequency-dependent decline with age, individuals with PD may exhibit more pronounced dysfunction and likely reflecting alpha-synuclein deposition in brainstem vestibular nuclei and connected regions. However, the concurrent presence of PD-specific vestibular changes vs. age-related alterations remains poorly understood.
Method: We recruited 46 PD and 26 age-matched normal controls. 17 PD (36.96%) and 7 controls (26.92%) were classified with PVP according to Barany Society criteria using multifrequency vestibular testing [1]. Balance assessment was conducted using the modified Romberg test and inertial sensors. All patients underwent dynamic gait and balance evaluation using the abbreviated Balance Evaluation Systems Test (MiniBESTest) total score and its four functional domain sub-scores (anticipatory postural control, reactive postural control, dynamic gait, and sensory integration). We compared inertial sensor measures and MiniMiniBESTest scores between PD patients without PVP and controls without PVP, and between PD patients with PVP and controls with PVP. T-tests were employed for these comparisons.
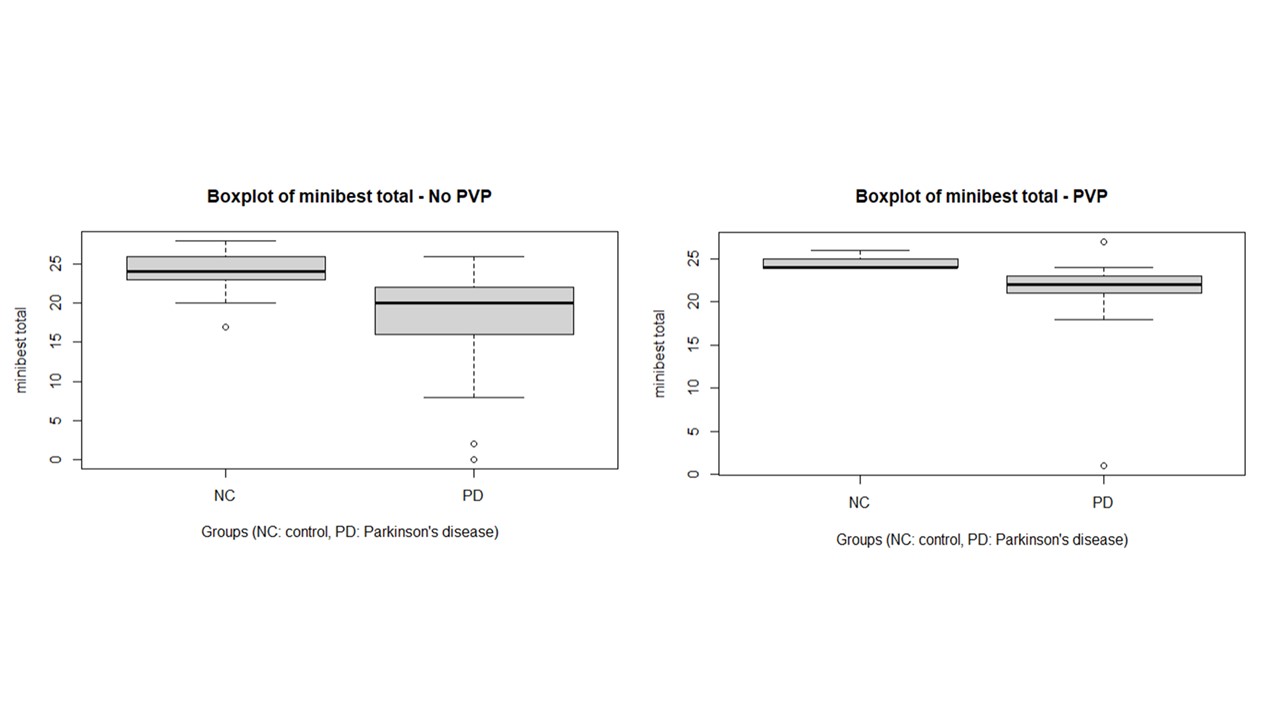
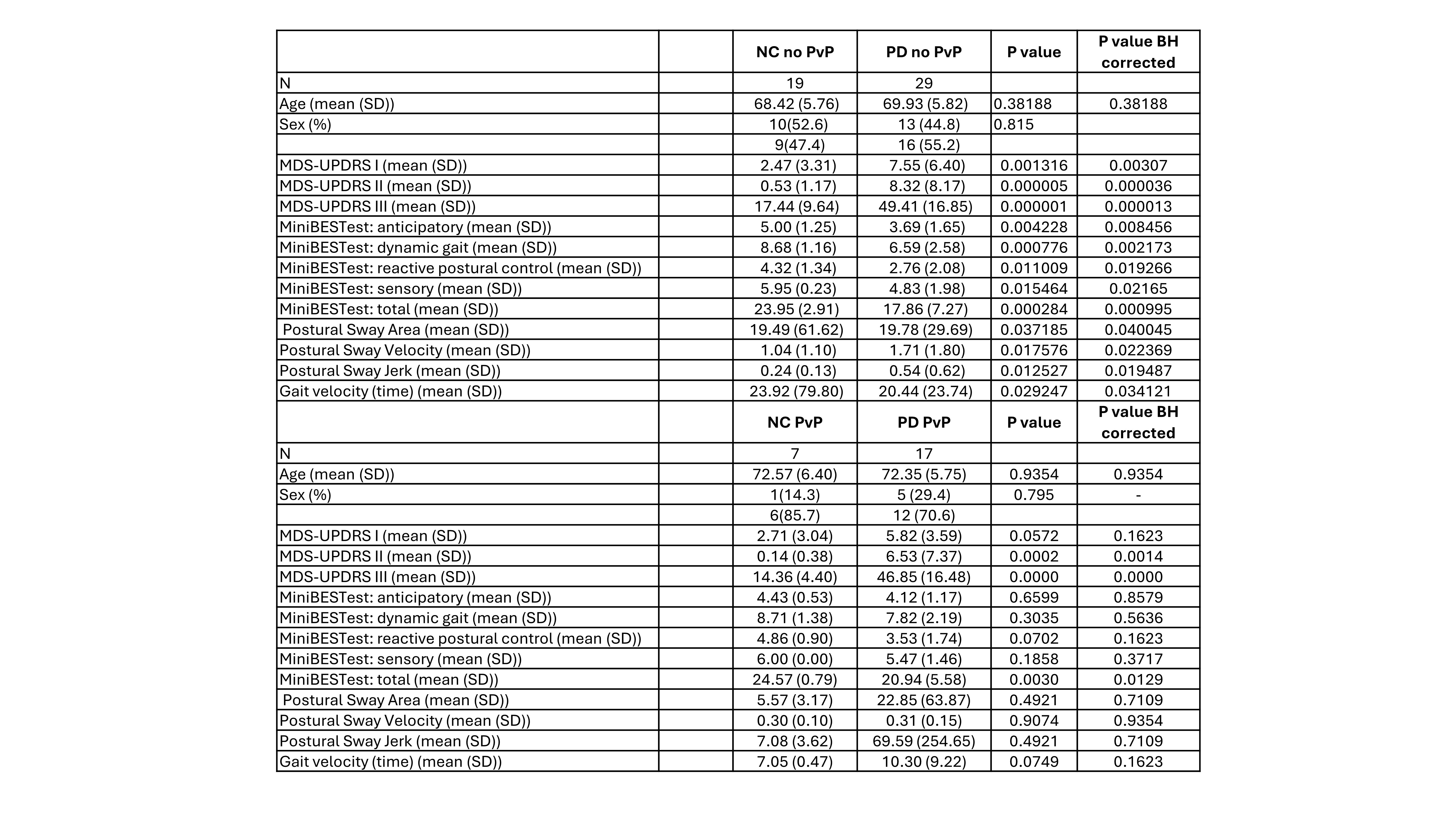
Results: PD patients without PVP exhibited significantly lower scores in MiniBESTest subcomponents and total scores, surviving multiple corrections, compared to controls without PVP [Table 1]. inertial sensor measures showed significant differences between the groups, with PD patients without PVP demonstrating greater and faster sway. In contrast, PD patients with PVP showed significantly lower scores in the MiniBESTest total score than controls with PVP [Figure 1].
Conclusion: These findings suggest that dynamic gait and balance, assessed through a simple test such as the MiniBESTest, could be a valuable tool for distinguishing PVP in PD from that in older NC persons. Furthermore, they imply greater vestibular involvement of the central nervous system in PD with PVP compared to the non-PD older subjects with PVP.
Figure 1
Table 1
References: [1] Agrawal, Y., Van de Berg, R., Wuyts, F., Walther, L., Magnusson, M., Oh, E., Sharpe, M., Strupp, .M. (2019). Presbyvestibulopathy: Diagnostic criteria Consensus document of the classification committee of the Bárány Society. Journal of Vestibular Research, 29(4), 161-170
To cite this abstract in AMA style:
G. Carli, D. Mccaslin, T. Brown, S. David, J. Barr, R. Vangel, A. Luker, C. Pongmala, K. Kerber, N. Bohnen. Exploring Vestibulopathy in PD: Distinguishing PD from Age-related Presbyvestibulopathy via Dynamic Gait and Balance Assessment [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/exploring-vestibulopathy-in-pd-distinguishing-pd-from-age-related-presbyvestibulopathy-via-dynamic-gait-and-balance-assessment/. Accessed July 1, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/exploring-vestibulopathy-in-pd-distinguishing-pd-from-age-related-presbyvestibulopathy-via-dynamic-gait-and-balance-assessment/