Session Information
Date: Thursday, June 8, 2017
Session Title: Parkinson’s Disease: Clinical Trials, Pharmacology And Treatment
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: Assess the ways in which decision support tools and directional leads are affecting DBS programming.
Background: The typical approach to DBS programming has changed little since this therapy was introduced: a monopolar review followed by exploration of bipolar settings if needed. This approach is limiting for several reasons. First, the amount of time required to perform a monopolar review increases with the number of electrode contacts, and this problem is compounded by the large number of possible bipolar or multipolar settings available on directional leads. Hence, it is worthwhile to explore new approaches to DBS programming that reduce the amount of time and complexity, and could be used by non-experts. We are currently conducting a two-phase clinical trial to evaluate a mobile decision support for DBS programming that is being used by experts as well as home health nurses.
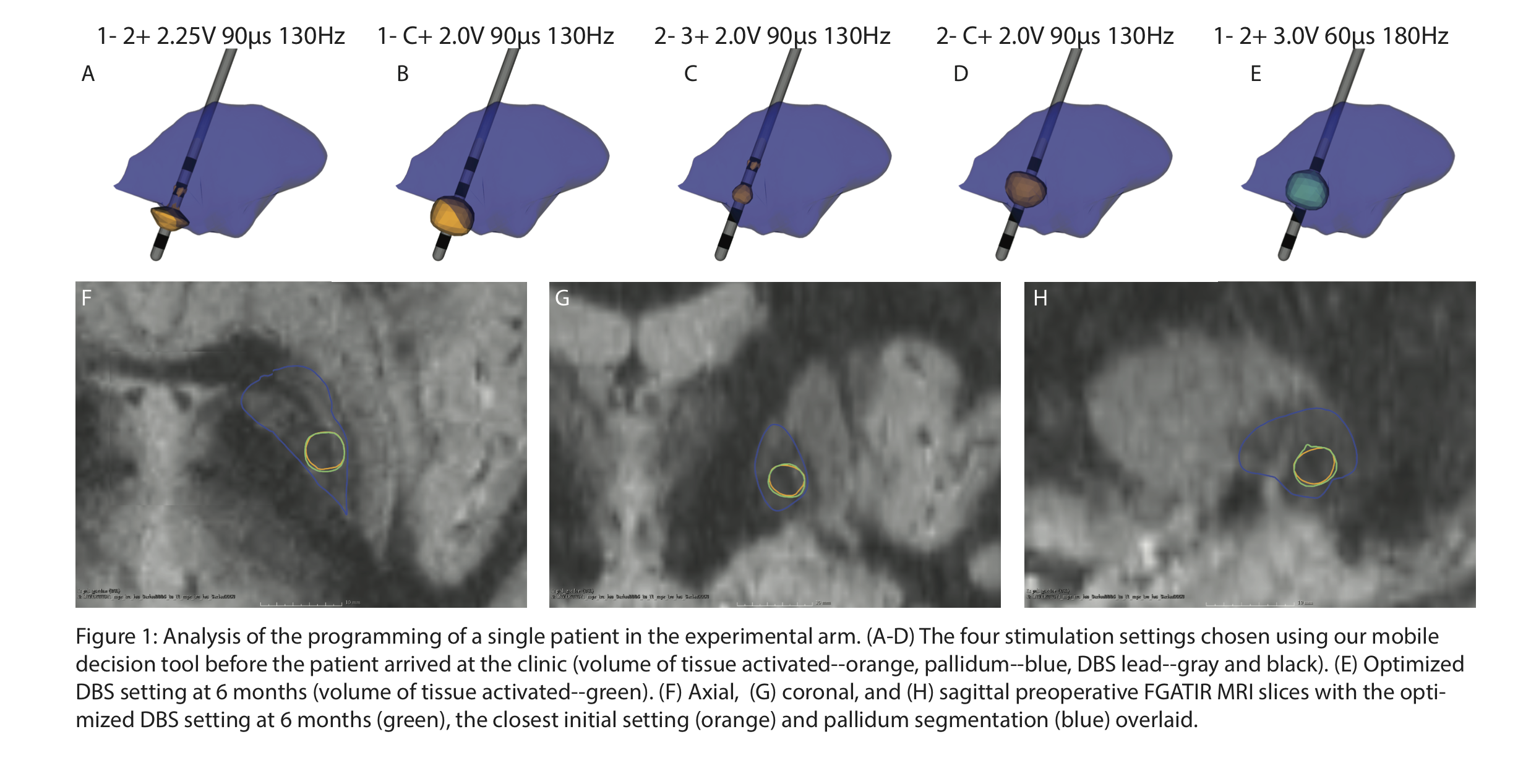
Methods: Patient specific models of DBS were generated using previously published methods [1] to predict the volume of tissue activated for a wide range of settings. Computational models are delivered to the DBS programming nurse via on an iPad decision support system; these models are reviewed before each patient’s initial programming visit in lieu of doing a monopolar review. The DBS programming nurse determines four electrode configurations from the model and starts the programming process from those settings rather than the thresholds determined by the monopolar review. This is an ongoing study and clinical outcomes are not yet available. Here we report our preliminary observations on the use of our programming platform for four Parkinson’s disease subjects who were followed for 6 months post-operatively. [figure1]
Results: For each of the four patients, the electrode configuration chosen after 6 months used either the same contact chosen during their initial visit or an adjacent contact, signifying at least a 25% reduction in the parameter space of possible contacts. Two of the four patients had their optimal electrode configuration as a setting determined from the iPad model during initial programming.
Conclusions: The current paradigm for DBS programming is likely to be untenable given the increasing complexity of the implanted systems and diminishing time available for DBS programming. Our preliminary results suggest that effective settings can be chosen using decision support tools that, at the very least, obviate the need for a monopolar review.
References: [1] Butson, Christopher R., et al. “Probabilistic analysis of activation volumes generated during deep brain stimulation.” Neuroimage 54.3 (2011): 2096-2104.
To cite this abstract in AMA style:
G. Duffley, A. Schiewe, B. Lutz, J. Krüger, M. Okun. How will new technology change deep brain stimulation programming? [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/how-will-new-technology-change-deep-brain-stimulation-programming/. Accessed July 15, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/how-will-new-technology-change-deep-brain-stimulation-programming/