Objective: To measure the impact of intensive multimodal neurorehabilitation in patients with moderately advanced with Parkinson’s disease (PD)
Background: Dedicated neurorehabilitation is an essential part of the multidisciplinary care regimen for PD patients [1,2,3]. Intensive multimodal programs may be especially efficacious for motor and non-motor symptoms in moderately advanced patients, who are at higher risk of falling and losing independent function [4,5]. Few studies have been conducted in an inpatient setting, where multi-modal therapies and tailored pharmacological intervention can be personalized. Here we present initial functional and quality of life outcomes for patients admitted to a dedicated Parkinson’s Rehabilitation Unit.
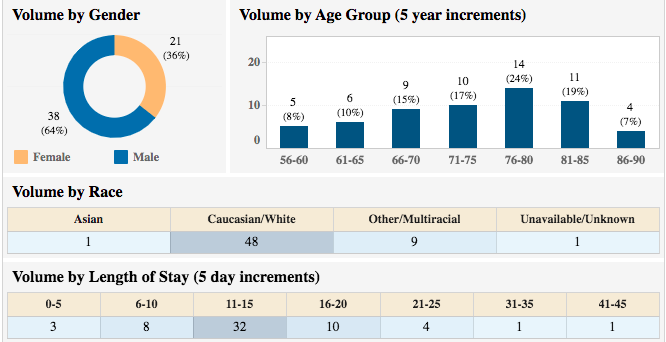
Method: 59 patients with PD (H&Y Stage 3-4) were admitted to a dedicated neurorehabilitation Parkinson’s unit. [table 2] Admission criteria included loss of independence in key life functions and falls within the past year. Patients participated in a structured inpatient, personalized multidisciplinary program with an emphasis on physical, occupational, and speech therapies. The patients were also followed by Movement Disorders specialists, who tailored pharmacotherapy. Average length of stay was 14.5 days. The following scales were administered at both admission and discharge: Beck’s Depression Inventory (BDI), Sleep Scale (PDSS), Timed Up and Go (TUG) Test, Vocal Volume, Parkinson’s Disease Questionnaire (PDQ-39). The statistical methods utilized were two-sample paired t-tests and correlation analyses.
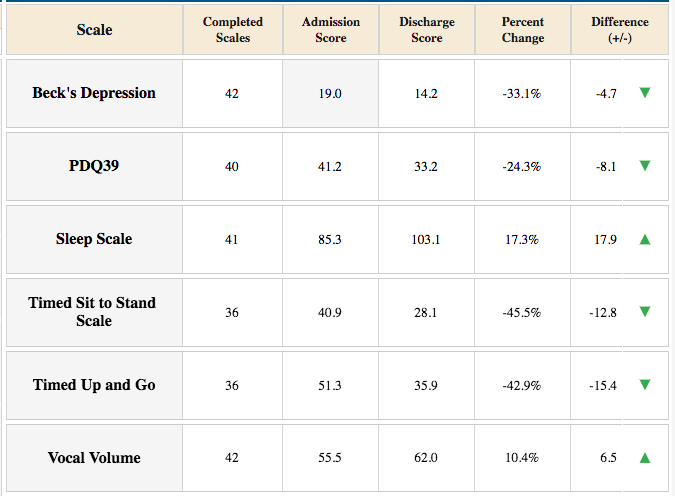
Results: [table 1] BDI scores decreased from M=19.04 (SD+10.89) to M=14.23 (SD+9.48); t(41)=4.39, p≤0.05; PDSS scores decreased from M=85.56 (SD+25.50) to M=103.12 (SD+27.09); t(40)=5.27, p≤0.05; TUG scores decreased from M=51.87 (SD+31.86) to M=34.11 (SD+15.00), t(35)=3.52, p≤0.05; Vocal volume scores increased from M=55.60 (SD+4.96) to M=61.98 (SD+6.26); t(41)=11.66, p≤0.05; PDQ-39 scores increased from M=41.56 (SD+17.51) to M=32.86 (SD +18.18); t(39)=6.46, p≤0.05. Regression analyses showed a strong correlation of sleep (p=0.0021) and mood (p=0.0003) with PDQ-39.
Conclusion: Neurorehabilitation is integral in the treatment of PD as medications have limited efficacy in advanced stages of this progressive disease. Although uncontrolled, the study indicates that individualized, multi-modal rehabilitation intervention in moderately advanced PD can have a global effect on function.
References: [1] Keus, S., Munneke, M., Graziano M, et al. (2014). European Physiotherapy Guideline for Parkinson’s Disease. KNGF/ParkinsonNet; https://www.parkinsonnet.nl/app/uploads/sites/3/2019/11/eu_guideline_parkinson_guideline_for_pt_s1.pdf
[2] Tomlinson, C. L., Patel, S., Meek, C., et al. (2012) Physiotherapy intervention in Parkinson’s disease: systematic review and meta analysis. BMJ. 345:e5004
[3] Ekker, M. S., Janssen, S., Nonnekes, J., Bloem, B. R., & De Vries, N. M. (2016). Neurorehabilitation for Parkinson’s disease: future perspectives for behavioural adaptation. Parkinsonism & related disorders, 22, S73-S77
[4] Lang, A. E. (2020) The evidence for multidisciplinary care in Parkinson’s disease. Expert Rev Neurother. 20(6):539-549
[5] Meloni, M., Saibene, F. L., Di Tella, S., Di Cesare, M., Borgnis, F., Nemni, R., & Baglio, F. (2021). Functional and Cognitive Improvement After an Intensive Inpatient Multidisciplinary Rehabilitation Program in Mild to Severe Parkinson’s Disease: A Retrospective and Observational Study. Frontiers in neurology, 12, 626041
To cite this abstract in AMA style:
P. Moondra, A. Di Rocco, L. Rubin, C. Claro, A. Persaud, M. Mccrossin, A. Hernandez, D. Barreto, K. Schlosser, E. Stack, P. Fischetti, J. Yu, D. Green, L. Ptarcinski, K. Greco, G. Fequiere, C. Francavilla, B. Rubin, M. Tursi, J. Colton. Intensive Multimodal Rehabilitation Intervention for Moderately Advanced Parkinson’s Disease [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/intensive-multimodal-rehabilitation-intervention-for-moderately-advanced-parkinsons-disease/. Accessed July 15, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/intensive-multimodal-rehabilitation-intervention-for-moderately-advanced-parkinsons-disease/