Category: Parkinson's Disease: Neuroimaging
Objective: Determine whether enlarged perivascular spaces (ePVS) in Parkinson’s disease (PD) is associated with worsening motor symptoms and disease progression.
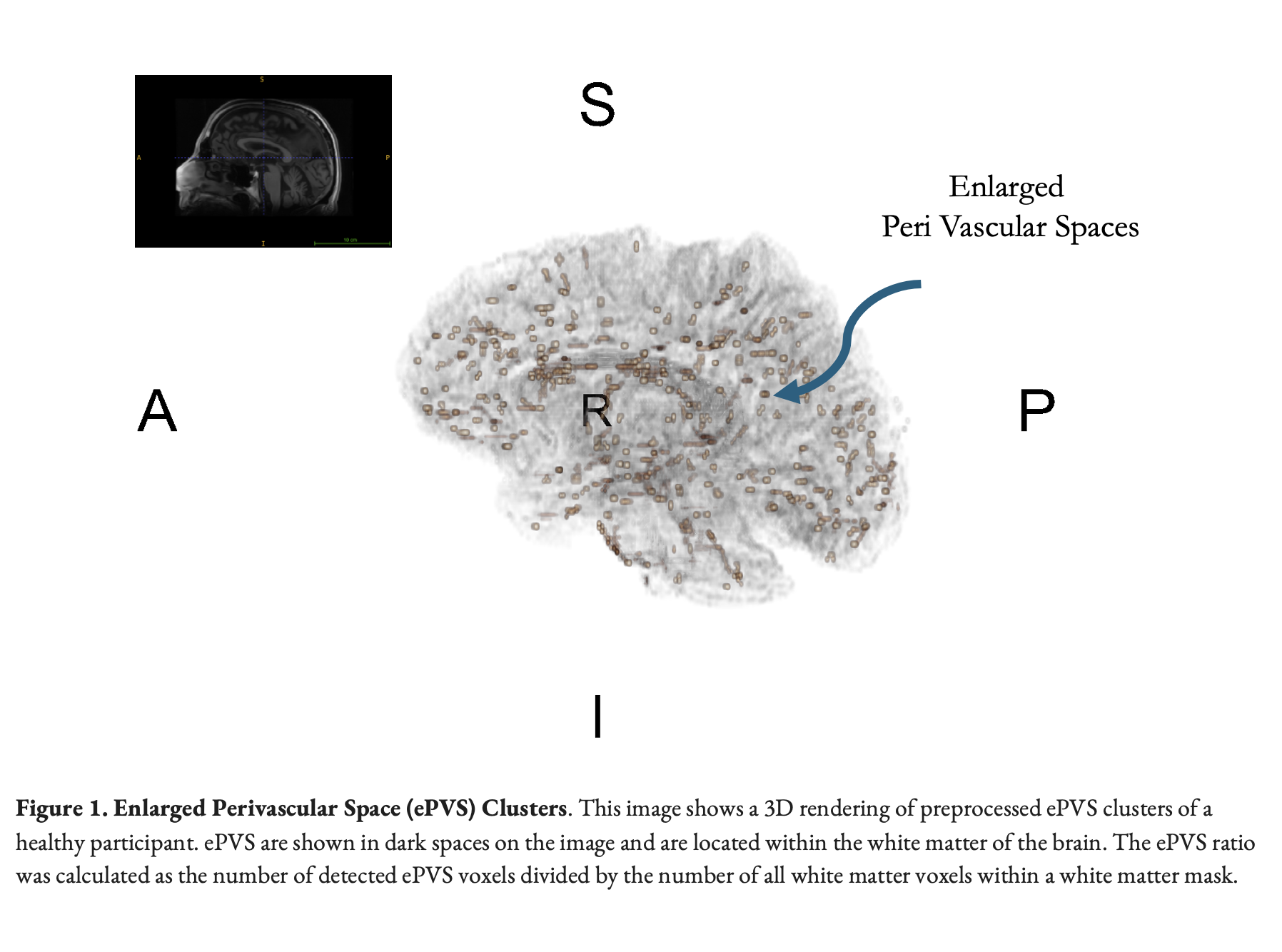
Background: PVS are fluid-filled channels surrounding brain vessels [1]. Enlarged PVS are linked to aging and neurodegeneration [2]. Advanced MRI techniques can be used to quantify ePVS, but their association with symptoms in PD remains unclear.
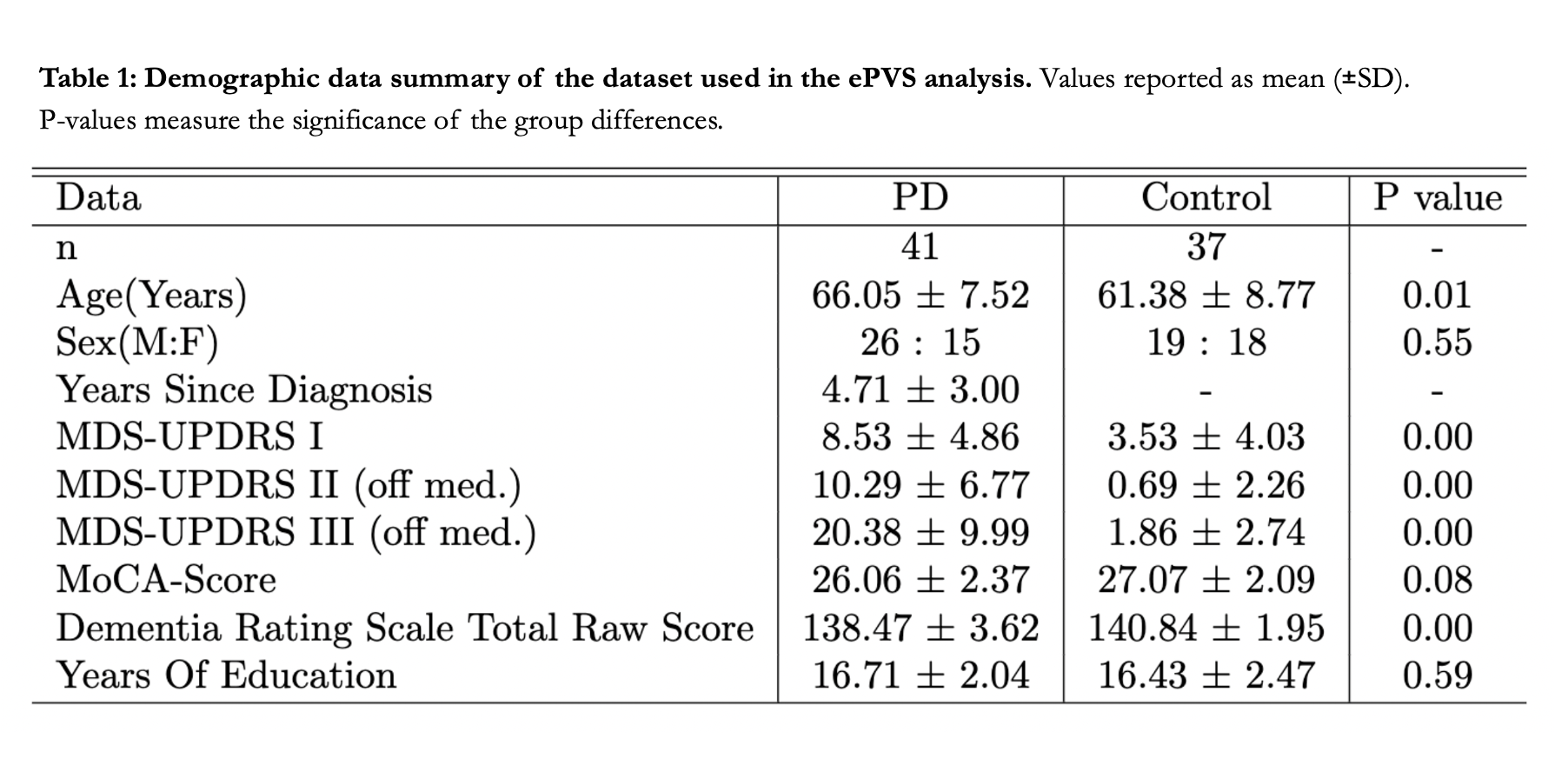
Method: Forty-one mild/moderate PD and 36 healthy control participants underwent structural MRI scans, comprehensive motor assessments using the MDS-UPDRS and the Scale for the Assessment and Rating of Ataxia [Table1]. MDS-UPDRS part I, II, III were performed on and off dopaminergic medications. Preprocessed 3 Tesla GE T1 and T2 weighted images were combined to enhance the contrast of PVS [3]. By applying a Frangi filter [4] to T1w, T2w images we generated vesselness maps for perivascular space (PVS) delineation. Thresholding these maps created a binary mask of ePVS, allowing for automated quantification of ePVS volume [5] [Figure1]. The ePVS ratio was calculated as the total ePVS volume divided by the total white matter volume within a white matter mask.
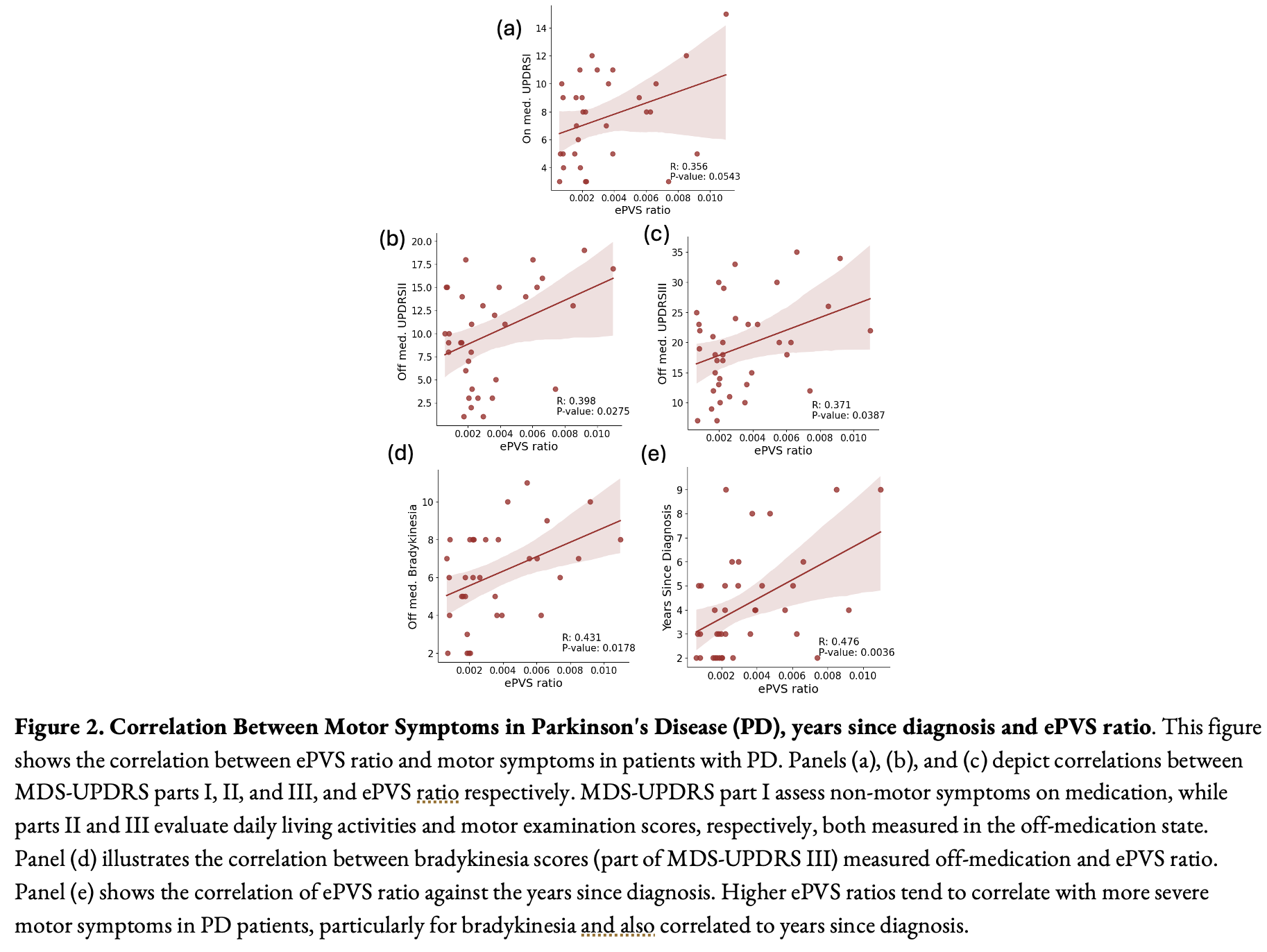
Results: PD patients did not exhibit a significant difference (p>0.52) in ePVS ratio compared to controls. However, within PD patients, a higher ePVS ratio correlated with both years since diagnosis (r=0.48, p=0.003) and motor symptom severity (UPDRS-I, II, III), particularly bradykinesia in the off-medication state (r=0.43, p=0.018) [Figure2]. By contrast, the ePVS ratio did not show a significant relationship with age (r=0.10, p=0.57), fine finger movement score (r=0.29, p=0.45) or ataxia (r=0.35, p=0.15) in the PD group [Figure3].
Conclusion: Our findings reveal a significant correlation between the ePVS ratio and motor severity scores in patients with PD, and notably, no correlation with general aging, fine finger movement, or ataxia. This suggests a potential association of ePVS as a marker for PD-specific motor dysfunctions, bridging the missing link with impaired waste clearance mechanisms in PD. Further research is warranted to explore the potential of ePVS as a biomarker for disease progression and therapeutic targets in PD. Support: AG081144, NS132101, NS115114, Michael J. Fox Foundation for Parkinson’s Research
Figure 3
Table 1
Figure 2
Figure 1
References: [1] Iliff JJ, Wang M, Liao Y, et al. A Paravascular Pathway Facilitates CSF Flow Through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid β. Sci Transl Med. 2012;4(147):147ra111. doi:10.1126/scitranslmed.3003748
[2] Ramirez J, Berezuk C, McNeely AA, Gao F, McLaurin J, Black SE. Imaging the Perivascular Space as a Potential Biomarker of Neurovascular and Neurodegenerative Diseases. Cell Mol Neurobiol. 2016;36(2):289-299. doi:10.1007/s10571-016-0343-6
[3] Younes K, Cobbigo Y, Tsuie T, et al. Divergent enlarged perivascular spaces volumes in early versus late age-of-onset Alzheimer’s disease. medRxiv. Published online 2023. doi:10.1101/2023.08.01.23293514
[4] Frangi AF, Niessen WJ, Vincken KL, Viergever MA. Multiscale vessel enhancement filtering. In: Wells WM, Colchester A, Delp S, eds. Medical Image Computing and Computer-Assisted Intervention — MICCAI’98. Springer; 1998:130-137. doi:10.1007/BFb0056195
[5] Sepehrband F, Barisano G, Sheikh-Bahaei N, et al. Image processing approaches to enhance perivascular space visibility and quantification using MRI. Sci Rep. 2019;9(1):12351. doi:10.1038/s41598-019-48910-x
To cite this abstract in AMA style:
D. Hemachandra, K. Younes, E. Peterson, J. Winer, Y. Cobbigo, H. Rosen, C. Young, T. Schulte, K. Poston, E. Müller-Oehring. MRI Visible Perivascular Spaces are Associated with Disease Duration and Severity in Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/mri-visible-perivascular-spaces-are-associated-with-disease-duration-and-severity-in-parkinsons-disease/. Accessed January 30, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/mri-visible-perivascular-spaces-are-associated-with-disease-duration-and-severity-in-parkinsons-disease/