Category: Ataxia
Objective: This study aimed to evaluate the various cognitive and psychiatric manifestations in patients with DCA.
Background: Degenerative cerebellar ataxias (DCA) are diseases with complex phenotypes, combined with gait abnormalities, incoordination, abnormalities of eye movements, and speech. The phenotype quite often includes, besides motor symptoms, neuropsychiatric manifestations.
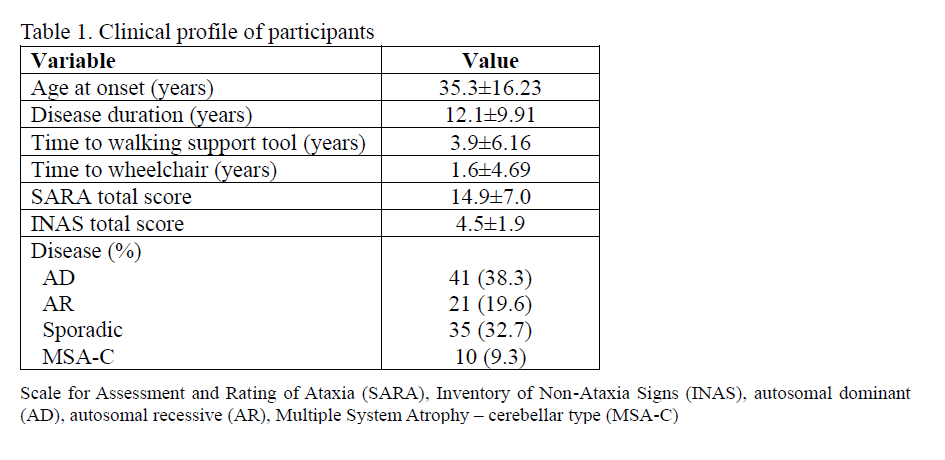
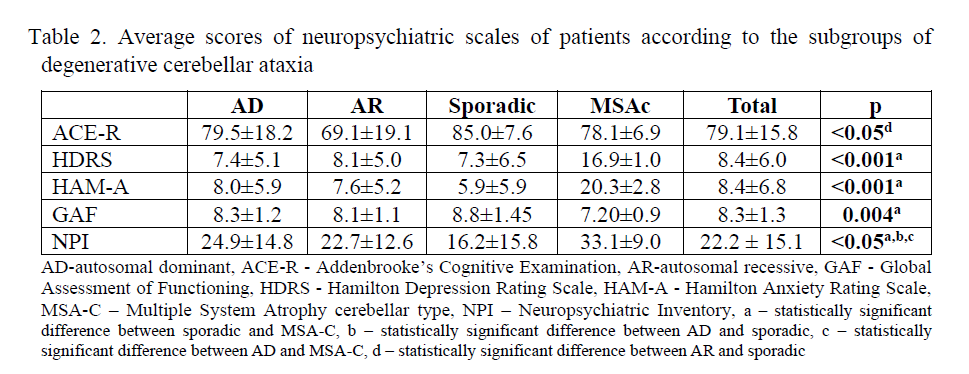
Method: We included a total of 107 patients with DCA. All patients were clinically evaluated using the Scale for the Rating and Assessment of Ataxia (SARA) and Inventory of Non-Ataxia Signs (INAS). For the assessment of cognitive functions and psychiatric manifestations Addenbrooke’s Cognitive Examination (ACE-R), Hamilton Depression Rating Scale (HDRS), Hamilton Anxiety Rating Scale (HAM-A), Global Assessment of Functioning (GAF) scale, and Neuropsychiatric Inventory (NPI) were used.
Results: The majority of patients had an inheritance of autosomal dominant cerebellar ataxia (38.3%) or were sporadic cases (32.7%), while autosomal recessive cerebellar ataxia (ARCA) and multiple system atrophy cerebellar type (MSA-C) were present in 19.6% and 9.3%, respectively. Table 1 presents clinical manifestations and the mean scores of SARA and INAS scales of the whole group of patients that are included in this study. Table 2 presents average scores of neuropsychiatric tests according to the patient’s subgroups of DCA with statistically significant differences between the subgroups. Patients with ARCA had statistically significant lower scores of ACE-R in regard to sporadic cases (p<0.05). It was shown that the SARA score had a statistically significant positive correlation with average scores of HDRS (r=0.349, p<0.01), HAM-A (r=0.214, p<0.01), NPI (r=0.455, p<0.01), while the negative correlation with GAF (r=0.439, p<0.01) in the total group of patients. INAS scores of the whole group of patients had a statistically significant positive correlation with NPI score, as well as, a negative correlation with GAF (r=-0.345, p<0.01). There was no statistically significant correlation between INAS analyzed with HDRS and HAM-A scores.
Conclusion: Our study has shown that besides the severity of motor symptoms, cognitive dysfunction and psychiatric symptoms present an important part of the clinical manifestations of DCA and should be assessed, especially in patients with autosomal recessive ataxias and MSA-C.
Table 1
Table 2
To cite this abstract in AMA style:
A. Milovanovic, O. Tamaš, G. Marić, M. Janković, M. Kostić, B. Salak đokić, E. Stefanova, N. Dragašević Mišković. Neuropsychiatric Manifestations in Patients with Degenerative Cerebellar Ataxias from Serbia [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/neuropsychiatric-manifestations-in-patients-with-degenerative-cerebellar-ataxias-from-serbia/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neuropsychiatric-manifestations-in-patients-with-degenerative-cerebellar-ataxias-from-serbia/