Category: Parkinsonism, Atypical: PSP, CBD
Objective: To evaluate the neuropsychiatric symptoms in patients with probable Progressive supranuclear palsy attended in reference centers of the Valle del Cauca, Colombia, between 2020 and 2024
Background: Progressive supranuclear palsy (PSP) is mainly characterized by parkinsonism, alterations in gait and stability, early falls and limitation of vertical eye movements, however its different phenotypes include multiple non-motor symptoms and neuropsychiatric impairment that tend to be less evaluated. [1].
Method: Patients with probable PSP, were evaluated with clinical assessment and motor and non-motor scales by a movement disorders neurologist, PSP phenotypes were classified by international criteria [1], and descriptive data are presented as mean ± standard deviation (SD) or frequencies where appropriate. Pearson’s correlation was analyzed between the PSP Rating Scale (PSPRS) and non-motor scales scores. A statistical significance was set at 0.05. Statistical analysis was performed with the SPSS statistical package (version 25; Chicago, IL, USA).
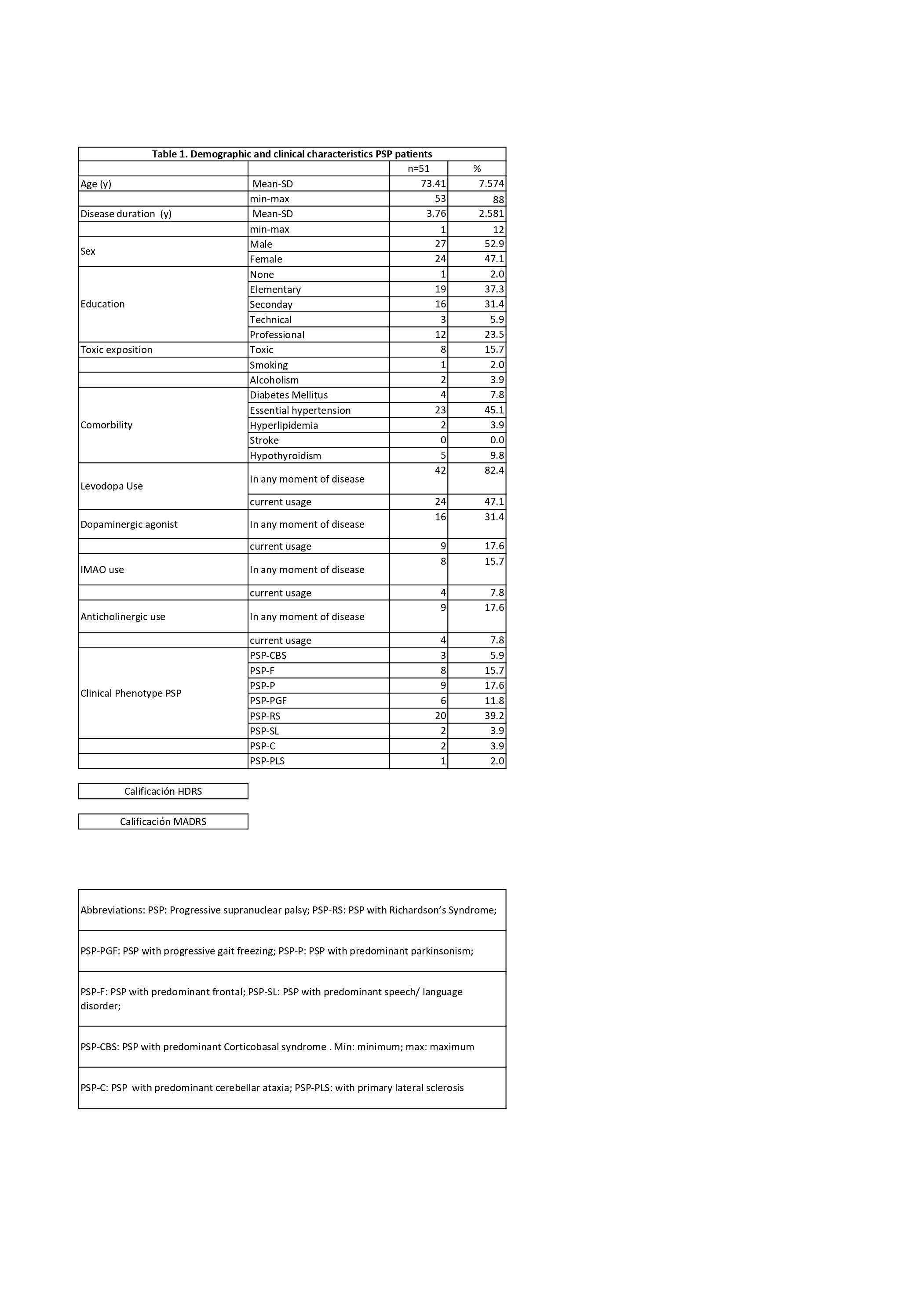
Results: 51 patients with probable PSP were included; 52.9% were male, the mean of symptoms duration was 3.7 years, and the main phenotype was PSP with Richardson’s Syndrome in 39.2% of patients; 37.3% has elementary education level , and 15% reported some degree of toxic exposure. 82.4% had received Levodopa in any moment of disease, and 47.1% currently use it . [Table 1].
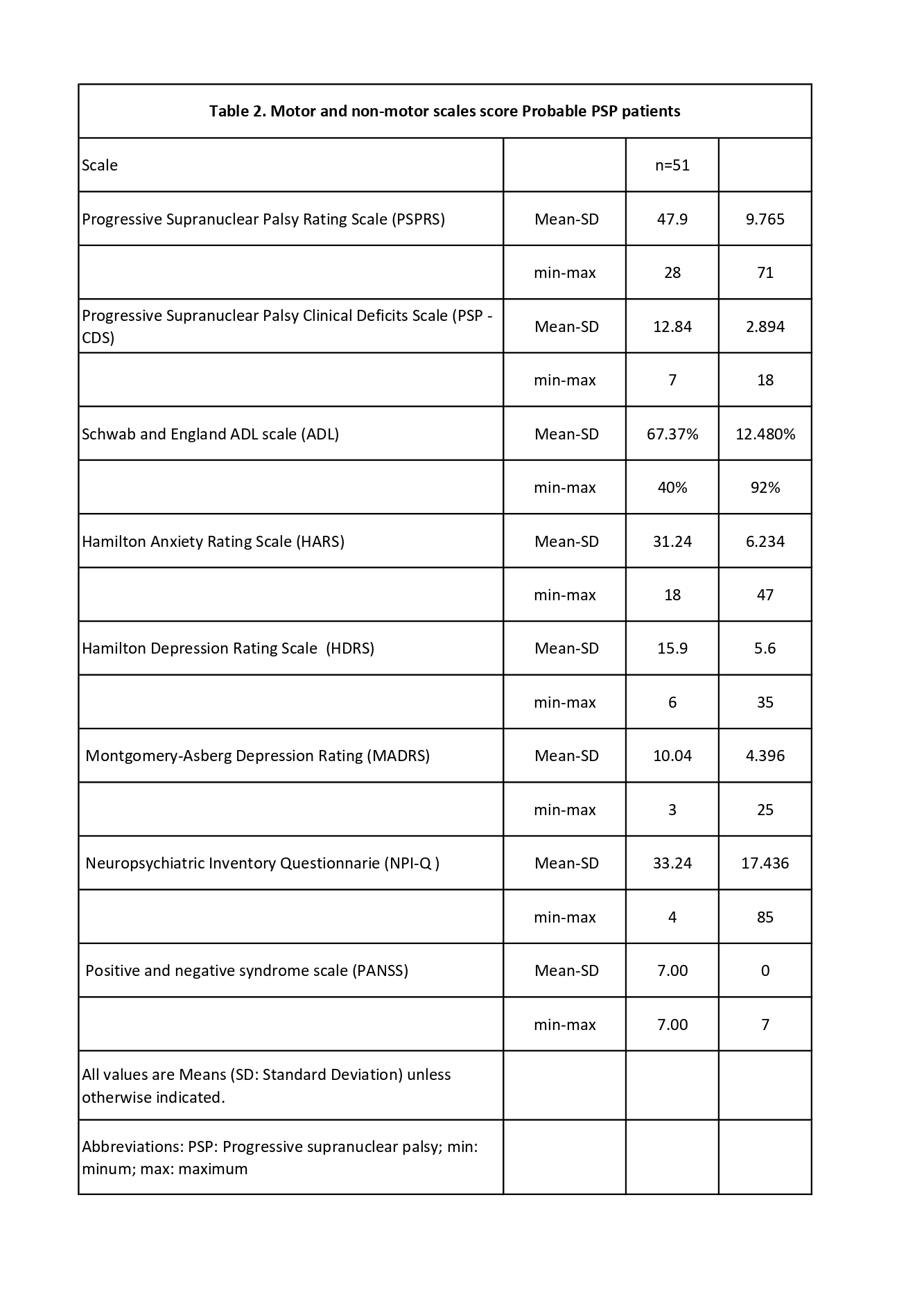
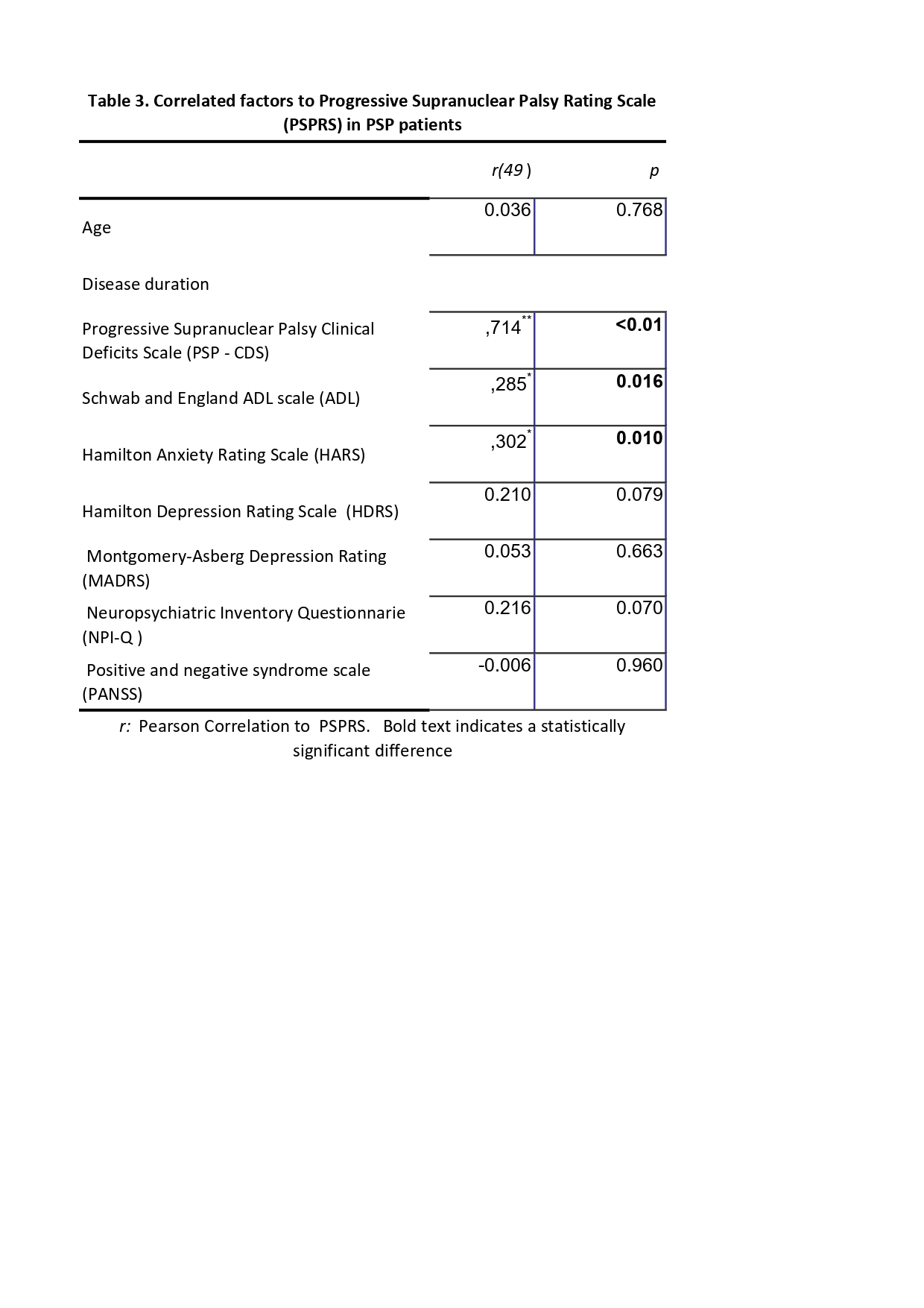
The Progressive Supranuclear Palsy Rating Scale (PSPRS) had a mean of 47.9 (SD 9.8), and the Schwab and England ADL Scale (ADL) of 67.37% (SD 12.5); All patients had a treatable anxiety disorder (Hamilton Anxiety Rating Scale -HARS), and 66.6% had moderate to severe depression (Hamilton Depression Rating Scale -HDRS), neuropsychiatric symptoms were common on the Neuropsychiatric Inventory Questionnaire (NPI- Q) but no psychotic features were found. [Table 2]. ADL and HARS were correlated with PSPRS score. [Table 3].
Conclusion: We found a high level of anxiety , depression and neuropsychiatric symptoms in the patients with probable PSP, but only anxiety correlated to motor compromise level, so we suggested evaluate neuropsychiatric symptoms in all the stages of the disease.
Tabla 1
Tabla 2
Tabla 3
References: 1. Höglinger, G. U., Respondek, G., Stamelou, M., Kurz, C., Josephs, K. A., Lang, A. E., Mollenhauer, B., Müller, U., Nilsson, C., Whitwell, J. L., Arzberger, T., Englund, E., Gelpi, E., Giese, A., Irwin, D. J., Meissner, W. G., Pantelyat, A., Rajput, A., van Swieten, J. C., … Litvan, I. (2017). Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Movement Disorders, 32(6), 853-84. https://doi.org/10.1002/mds.26987
2. Chaithra, S. P., Prasad, S., Holla, V. V., Stezin, A., Kamble, N., Yadav, R., & Pal, P. K. (2020). The Non-Motor Symptom Profile of Progressive Supranuclear Palsy. Journal of Movement Disorders, 13(2), 118-126. https://doi.org/10.14802/jmd.19066
To cite this abstract in AMA style:
V. Martínez-Villota, L. Ortega-Bolaños, C. Hurtado-Gonzalez. Neuropsychiatric symptoms in patients with probable Progressive supranuclear palsy in reference centers of Valle del Cauca- Colombia [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/neuropsychiatric-symptoms-in-patients-with-probable-progressive-supranuclear-palsy-in-reference-centers-of-valle-del-cauca-colombia/. Accessed July 12, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neuropsychiatric-symptoms-in-patients-with-probable-progressive-supranuclear-palsy-in-reference-centers-of-valle-del-cauca-colombia/