Category: Parkinson's Disease: Cognitive functions
Objective: To evaluate positional effects on cognitive performance and cerebral hemodynamics in Parkinson’s disease (PD) patients with and without orthostatic hypotension (OH).
Background: OH is a common manifestation of PD and is associated with both short-term and long-term cognitive impairment [1-5], yet the mechanism for this link is not well understood. A better understanding of the relationship between positional BP, cerebral hemodynamics, and cognition in PD is essential to reduce the risks of cognitive impairment.
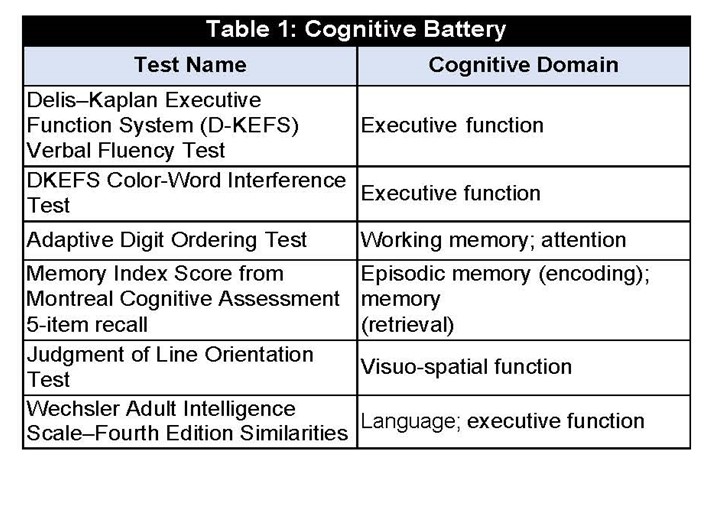
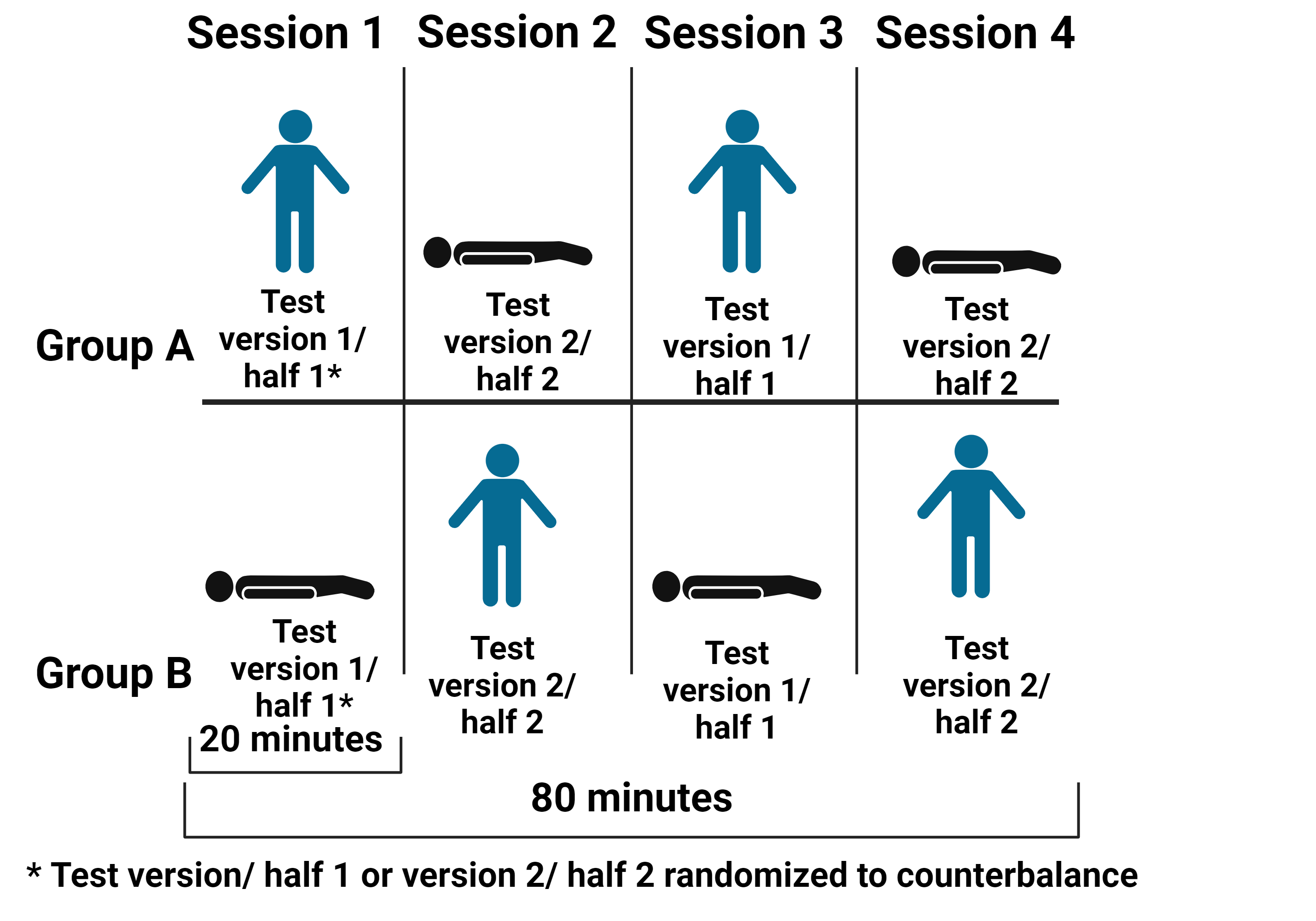
Method: We recruited PD patients (10 without OH (OH-), 7 with OH (OH+) (UCSD IRB # 210738) who completed a cognitive battery [table1] consisting of four consecutive sessions of cognitive testing in alternating positions (i.e., supine, upright) on a tilt table [figure1] while wearing functional near-infrared spectroscopy (NIRSport2, NIRx Medical Technologies LLC) to simultaneously measure cerebral hemodynamics. We compared cognitive performance in the supine and upright positions in the OH- and OH+ groups using independent t-tests. A linear mixed-effects regression model investigated the main and interaction effects of group (OH- and OH+) and position (supine vs. upright) on the dependent variables (cognitive performance and neural efficiency). Neural efficiency describes the mental effort (cerebral oxygenation) exerted in relation to cognitive performance, where lower neural efficiency indicates that the individual is utilizing high cognitive resources with lower performance; higher neural efficiency indicates that the individual is using less cognitive resources with higher performance6.
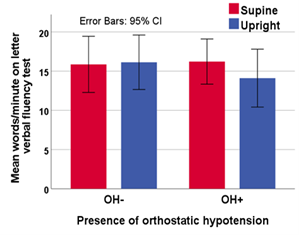
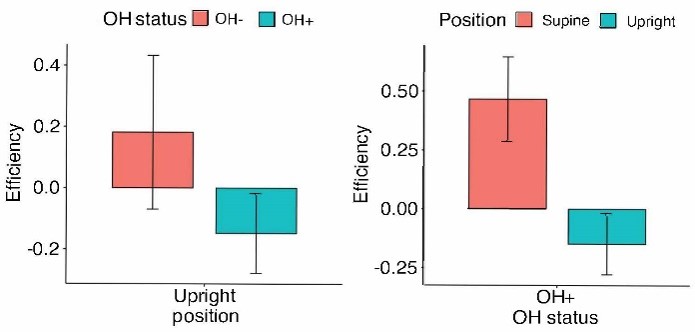
Results: The OH+ group performed worse on the Delis-Kaplan Executive Function System Verbal Fluency Test letter fluency test when upright (M=13.48 total correct responses, SD=3.62) compared to sitting/supine (M=15.81, SD=2.73, t(6)=3.63, p=0.015, 95% CI: (0.635, 4.030), d=1.27 [figure2]. Within the OH+ group (n=4), neural efficiency during the letter fluency test while upright was low (M=-0.09, SD= 0. 59) and efficiency was high while sitting/supine (M=0.82, D=0.67) (t(11)=2.37, p=0.037, 95% CI:(0.14, 2.07) [figure3] .
Conclusion: This preliminary data supports our hypothesis that individuals with PD with OH have impaired cerebral hemodynamic regulation associated with worse upright cognitive performance.
Table 1
Figure 1
Figure 2
Figure 3
References: 1. Centi, Justin, et al. “Effects of orthostatic hypotension on cognition in Parkinson disease.” Neurology 88.1 (2017): 17-24.
2. Sforza, Michela, et al. “Orthostatic hypotension acutely impairs executive functions in Parkinson’s disease.” Neurological Sciences 39 (2018): 1459-1462.
3. McDonald, Claire, Julia L. Newton, and David J. Burn. “Orthostatic hypotension and cognitive impairment in Parkinson’s disease: causation or association?.” Movement Disorders 31.7 (2016): 937-946.
4. Longardner, Katherine, et al. “Differential impact of individual autonomic domains on clinical outcomes in Parkinson’s disease.” Journal of neurology 269.10 (2022): 5510-5520.
5. Longardner, Katherine, Ece Bayram, and Irene Litvan. “Orthostatic hypotension is associated with cognitive decline in Parkinson disease.” Frontiers in neurology 11 (2020): 562726.
6. Bunce, Scott C., et al. “Implementation of fNIRS for monitoring levels of expertise and mental workload.” Foundations of Augmented Cognition. Directing the Future of Adaptive Systems: 6th International Conference, FAC 2011, Held as Part of HCI International 2011, Orlando, FL, USA, July 9-14, 2011. Proceedings 6. Springer Berlin Heidelberg, 2011.
7. Delis, Dean C., Edith Kaplan, and Joel H. Kramer. “Delis-Kaplan executive function system.” Assessment (2001).
To cite this abstract in AMA style:
K. Longardner, P. Reddy, K. Izzetoglu, I. Litvan. Orthostatic Hypotension is Associated with Worse Verbal Letter Fluency and Lower Neural Efficiency While Upright in Parkinson’s Disease: A Pilot Study [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/orthostatic-hypotension-is-associated-with-worse-verbal-letter-fluency-and-lower-neural-efficiency-while-upright-in-parkinsons-disease-a-pilot-study/. Accessed July 10, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/orthostatic-hypotension-is-associated-with-worse-verbal-letter-fluency-and-lower-neural-efficiency-while-upright-in-parkinsons-disease-a-pilot-study/