Category: Parkinson's Disease: Pathophysiology
Objective: To see if segmentation models of baseline DaT-SPECT striatal binding ratios (SBR) will predict freezing of gait (FoG) in Parkinson’s Disease over a 5, 7, and 10-year follow-up period in the Parkinson’s Progression Markers Initiative (PPMI) cohort.
Background: FoG is a source of significant morbidty in Parkinson’s disease[1]. Studies have shown SBR can predict FoG at 4 years[2]. We aimed to assess if SBR can predict FoG with a longer follow up.
Method: Logistic regression models of baseline DaT scans from PPMI participants who had no FoG at baseline were used to determine which of 4 possible segmentation models would accurately predict the likelihood of FoG at 5, 7, or 10-year clinical follow-up. The 4 models were: 1) Mean SBR of left and right caudate and putamen 2) SBR Hemispheres: Mean of left caudate and putamen, and right caudate and putamen, separately 3) Caudate and Putamen SBR: Mean of left and right caudate, and left and right putamen, separately 4) Individual Nuclei: left and right caudate and putamen individually. FoG was defined by the MDS-UPDRS 2.13 response. Models included sex, enrollment age, and symptom onset age as covariates. LASSO was then used to identify the most important variables.
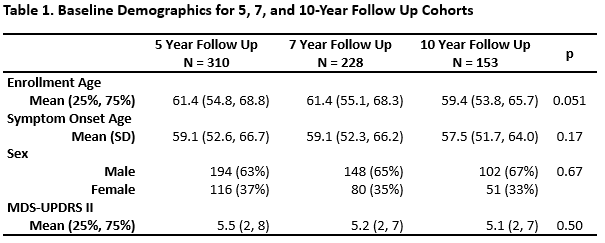
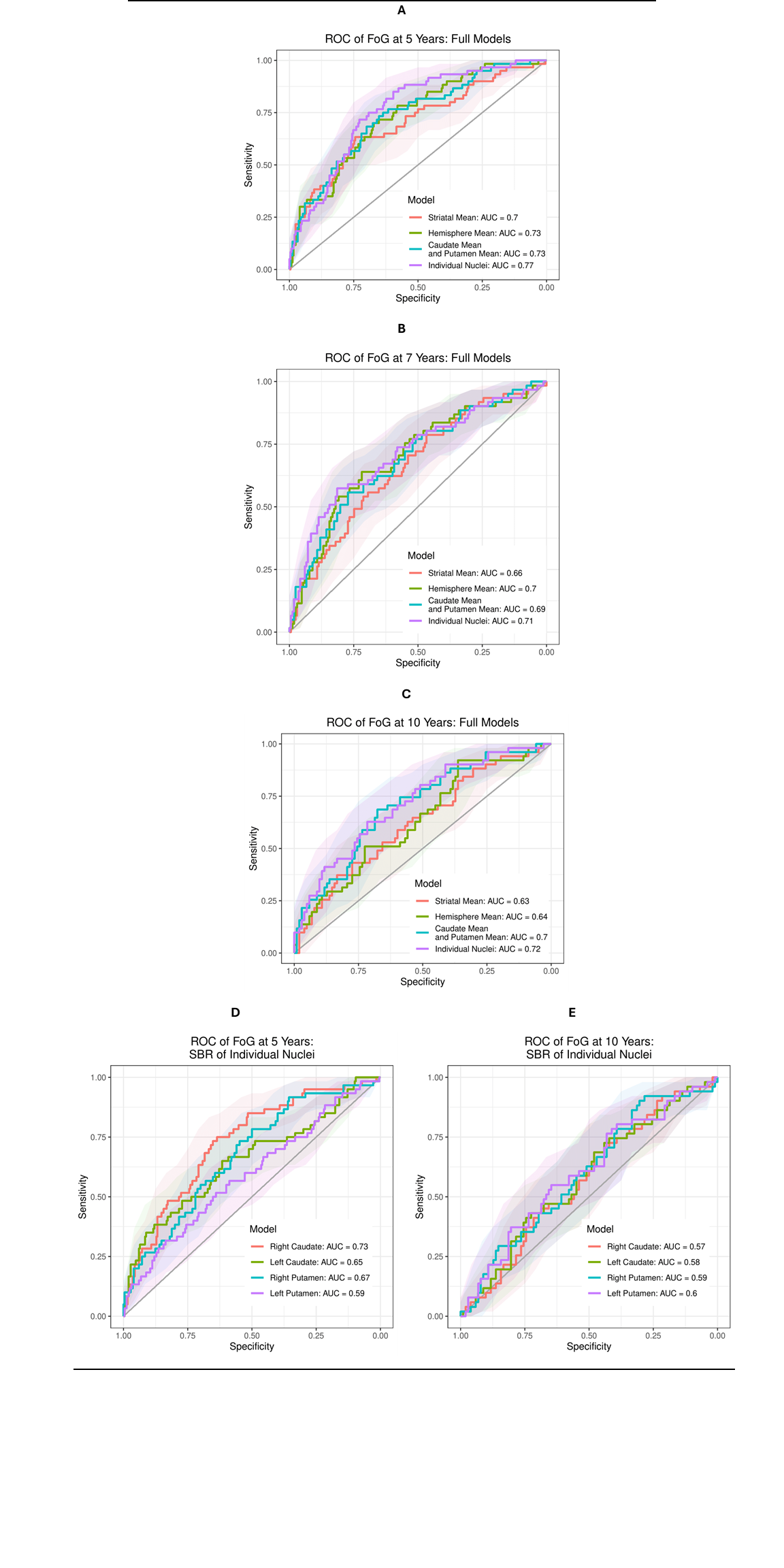
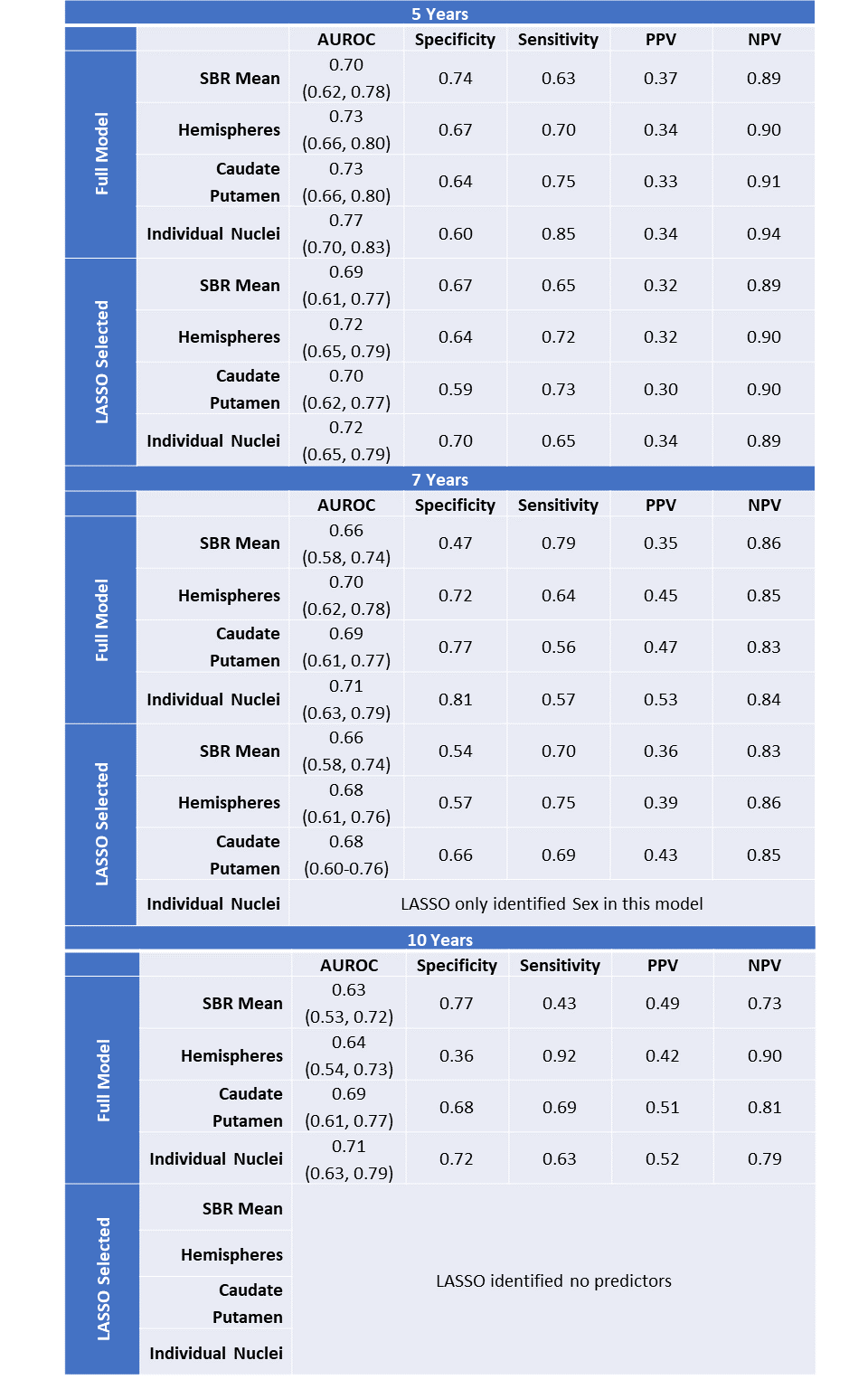
Results: Baseline demographics were not significantly different between 5, 7, and 10-year follow-up cohorts (Table 1). SBR at baseline was predictive of FoG at 5 (n=310) and 7 (n=228), but not 10-year (n=153) follow-up (Fig. 1). At 5 years, LASSO included the caudate and left hemisphere but excluded the putamen and right hemisphere in the respective models. The strongest prediction model was the Individual Nuclei model for 5-year follow up (AUROC=0.77). Separate logistic regressions assessing FoG at 5 years with each striatal nuclei individually observed that the right caudate was the most influential predictor (AUROC=0.73). At 7 years, LASSO included the putamen and left hemisphere and excluded the caudate and right hemisphere. Overall, models have high negative predictive value but poor positive predictive value (Table 2).
Conclusion: Our findings suggest that the individual nuclei model SBR may be the strongest predictor of FoG within 5 years. Attrition bias may have affected models at 7 and 10 years.
Table 1. Baseline Demographics
Figure 1. Logistic Regression ROCs
Table 2. Logistic Regression Model Results
References: 1. Perez-Lloret S, Negre-Pages L, Damier P, Delval A, Derkinderen P, Destée A, Meissner WG, Schelosky L, Tison F, Rascol O. Prevalence, determinants, and effect on quality of life of freezing of gait in Parkinson disease. JAMA Neurol. 2014 Jul 1;71(7):884-90. doi: 10.1001/jamaneurol.2014.753. PMID: 24839938.
2. Kim R, Lee J, Kim Y, Kim A, Jang M, Kim HJ, Jeon B, Kang UJ, Fahn S. Presynaptic striatal dopaminergic depletion predicts the later development of freezing of gait in de novo Parkinson’s disease: An analysis of the PPMI cohort. Parkinsonism Relat Disord. 2018 Jun;51:49-54. doi: 10.1016/j.parkreldis.2018.02.047. Epub 2018 Feb 28. PMID: 29523394.
To cite this abstract in AMA style:
J. Li, R. Rajmohan, J. Ruiz Tejeda, N. Phielipp. Predictive Accuracy of Baseline DaT-SPECT for Freezing of Gait at 5, 7, and 10-year Follow up in The PPMI Cohort [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/predictive-accuracy-of-baseline-dat-spect-for-freezing-of-gait-at-5-7-and-10-year-follow-up-in-the-ppmi-cohort/. Accessed July 10, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/predictive-accuracy-of-baseline-dat-spect-for-freezing-of-gait-at-5-7-and-10-year-follow-up-in-the-ppmi-cohort/