Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: To evaluate any dysphagia-signs in Parkinson’s disease (PD) with technique that is non-invasive, without-radiation-exposure and gives good soft-tissue contrast.
Background: Swallowing, a basic oromotor function for survival may have multifactorial involvement in PD which is difficult to evaluate clinically[1]. Available modalities videofluoroscopy (VFS) and flexible endoscopic evaluation of swallowing (FEES) are gold standard, but either have ionizing radiation, or invasive with limited soft-tissue details, so reliable technique is required for appropriate optimal management[2]. Magnetic Resonance Imaging (MRI) is non-invasive, without any radioactive exposure and dynamic (dMRI) with T2 weighting may evaluate normal-saline (NS) bolus giving soft tissue details[3].
Method: Study included 12 subjects with idiopathic PD (H&Y<2.5) and 6 healthy controls (HC) of age 45-72 yrs. Clinical assessment included swallowing (SDQ)[1], in neurodegeneration (CADN)[4]. Real-time dynamic MR (single slice 2-D sagittal) images acquired on 1.5T system (Aera, Siemens Healthcare, Germany) using 12H 4N and 4BFlex coils with T2 trueFISP (trufi-cine) sequence, FOV 230, TR162.54 ms, TE 1.27 ms, FA 44 degrees, ST 10mm, 19.2 fps and AT 8.53 minutes. Swallowing bolus - 10ml of normal saline (NS, 0.9%) delivered in mouth (rate 2ml/sec). Parameters analysed (i)jaw movement (ii)tongue positioning (iii)bolus transit (iv)velar closure (v)hyoid bone elevation (vi)epiglotic closure (vii)pharyngeal wave (viii)arytenoid movement (ix)residual bolus (x)spooling of saliva/ bolus.
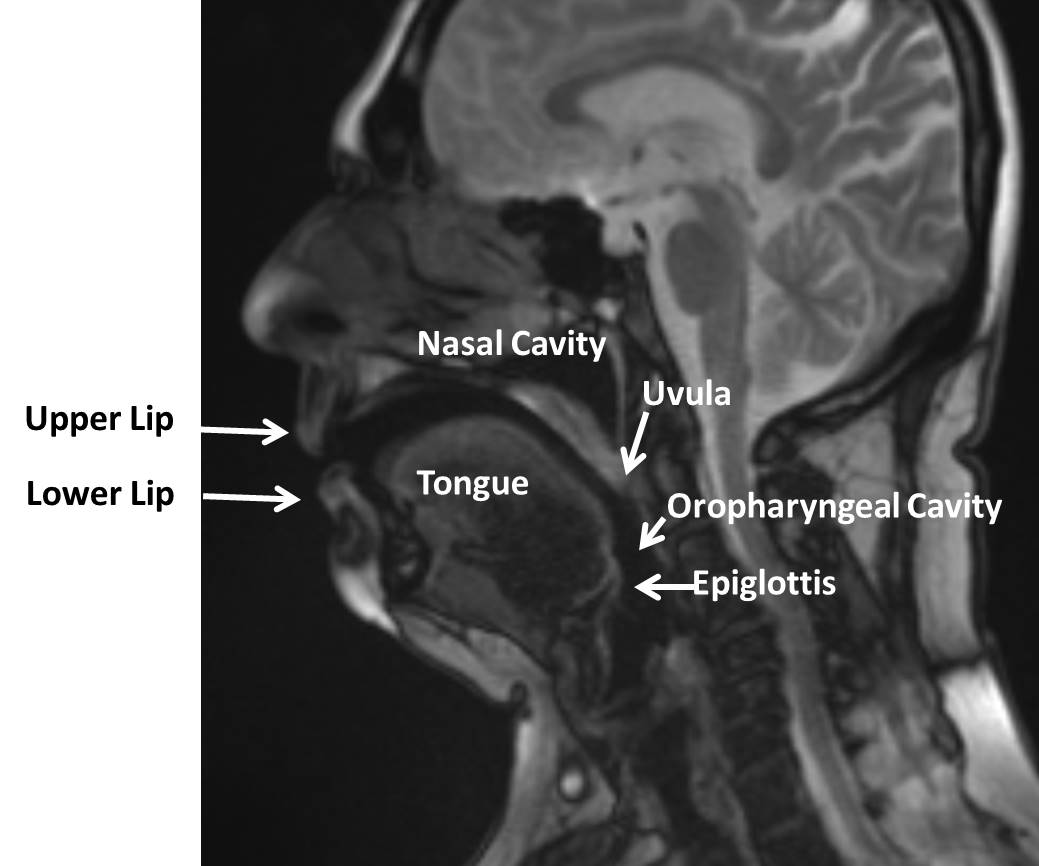
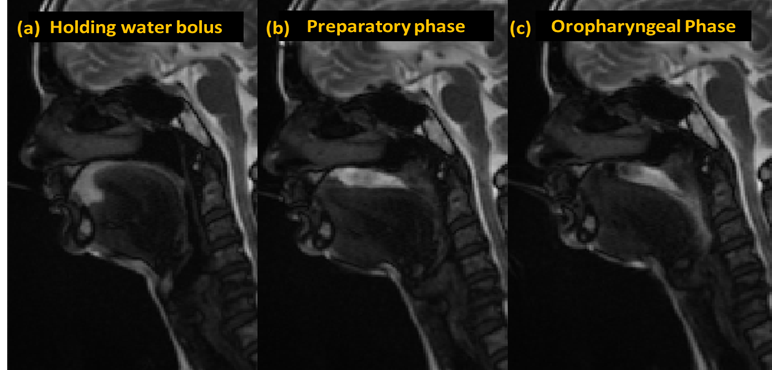
Results: None of the PD patient reported dysphagia signs subjectively. On clinical assessments (SDQ/CADN) none of the subject scored positive signs of dysphagia or indication for further diagnostic investigation. On dMRI PD patients as group had significant difference in preparatory (bolus wave), oral (tongue, velar posture), oropharyngeal (hyoid-movement, transit-time, bolus-residue) and oesophageal (arytenoid movement) phases.Figure-1: Anatomical Landmarks important in Swallowing Assessment [Figure1]Figure-2: Swallowing Mechanism in PD subject: (a) Holding water bolus (10ml of saline NS 0.9%) in oral cavity; (b) Tongue and bolus position in preparatory phase; (c) Transit of bolus in oropharyngeal phase [Figure2].
Conclusion: Dynamic MRI is a reliable clinical technique with good soft-tissue details for swallowing assessments. It detects early dysphagia signs in PD.
References: [1]Manor Y, Giladi N, Cohen A, Fliss DM, Cohen JT. Validation of a swallowing disturbance questionnaire for detecting dysphagia in patients with Parkinson’s disease. Mov Disord. 2007;22(13):1917-21 [2]Hashimoto H, Hirata M, Takahashi K, Kameda S, Katsuta Y, Yoshida F, Hattori N, Yanagisawa T, Palmer J, Oshino S, Yoshimine T, Kishima H. Non-invasive quantification of human swallowing using a simple motion tracking system. Sci Rep., 2018;8(1):5095. [3]Tanaka T, Oda M, Nishimura S, Kito S, Wakasugi-Sato N, Kodama M, Kokuryo S, Habu M, Miyamoto I, Yamashita Y, Aso A, Sadasue K, Nagashima R, Tominaga K, Yoshioka I, Morimoto Y. The use of high-speed, continuous, T2-weighted magnetic resonance sequences and saline for the evaluation of swallowing. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(4):490-496 [4]Vogel AP, Rommel N, Sauer C, Horger M, Krumm P, Himmelbach M, Synofzik M. Clinical assessment of dysphagia in neurodegeneration (CADN): development, validity and reliability of a bedside tool for dysphagia assessment. J Neurol. 2017; 264(6):1107-1117
To cite this abstract in AMA style:
SG. Gudwani, PU. Upadhyay, KS. Sharma, RS. Sagar, SSK. Kumaran, RKD. Dhamija. Swallowing assessment in Parkinson’s Disease using Dynamic Magnetic Resonance Imaging (dMRI) [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/swallowing-assessment-in-parkinsons-disease-using-dynamic-magnetic-resonance-imaging-dmri/. Accessed March 1, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/swallowing-assessment-in-parkinsons-disease-using-dynamic-magnetic-resonance-imaging-dmri/