Objective: To study various non-motor symptoms in idiopathic dystonia patients using validated scales.
Background: Dystonia is a hyperkinetic movement disorder. There has been a recent interest in understanding the various non-motor symptoms. A proper understanding of these non-motor symptoms will help in developing appropriate therapeutic strategies.
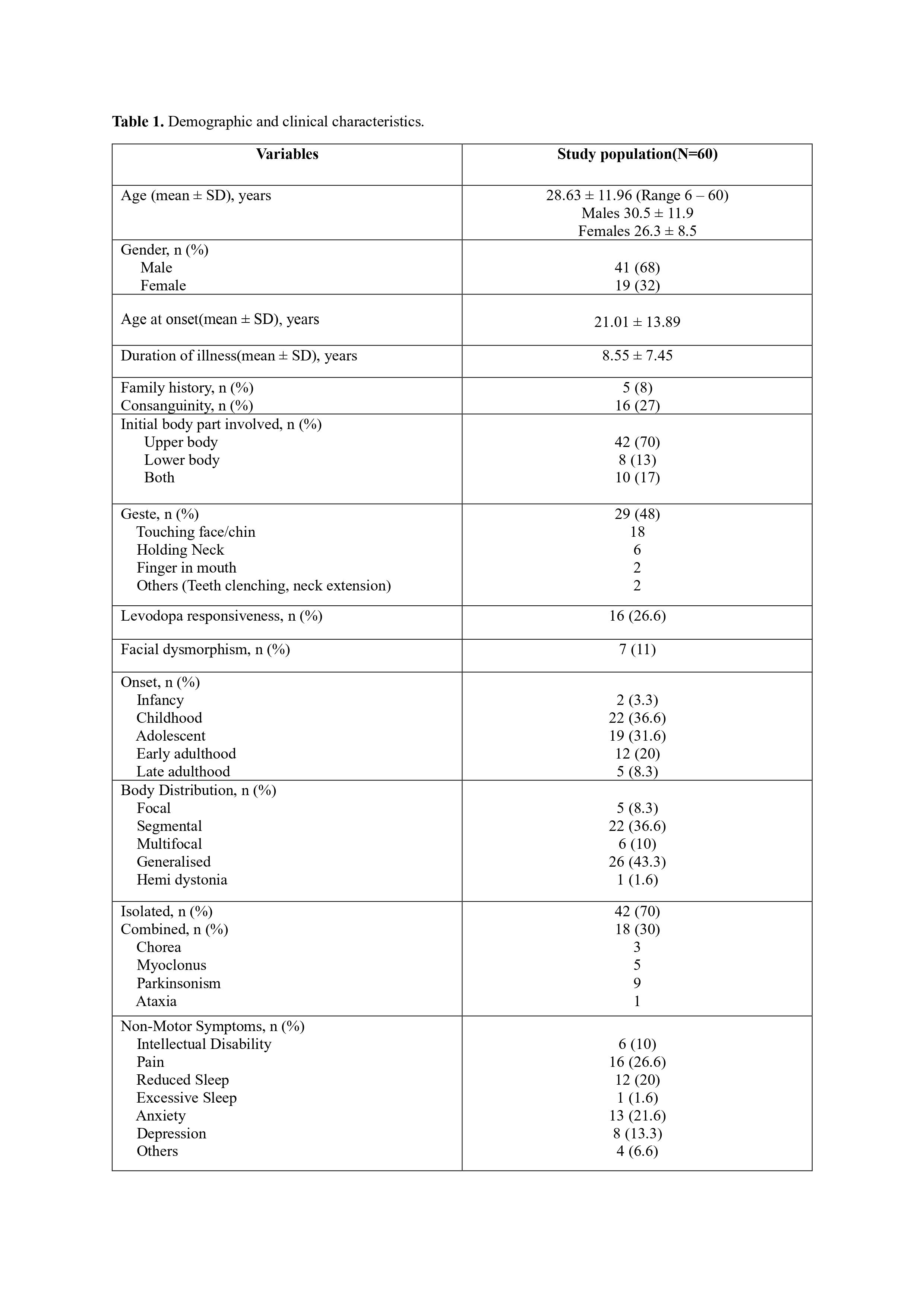
Method: Sixty idiopathic dystonia patients participated in a cross-sectional study at NIMHANS, Bengaluru. Approved by the Institute Ethics Committee, the study required written consent and adhered to inclusion/exclusion criteria. Demographics were noted, and motor severity assessed using BFMDRS and UDRS. Various validated scales measured non-motor symptoms, including RBDSQ, ESS, PSQI, HADS-A, HADS-D, MoCA, WHO-QoL, Caregiver burden was gauged using the Zarit scale.
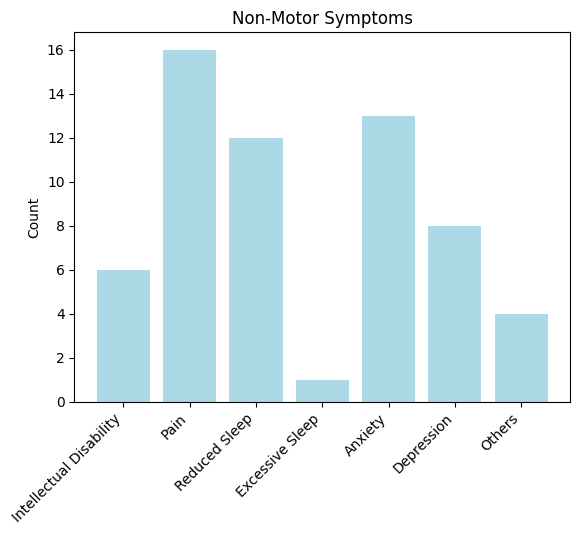
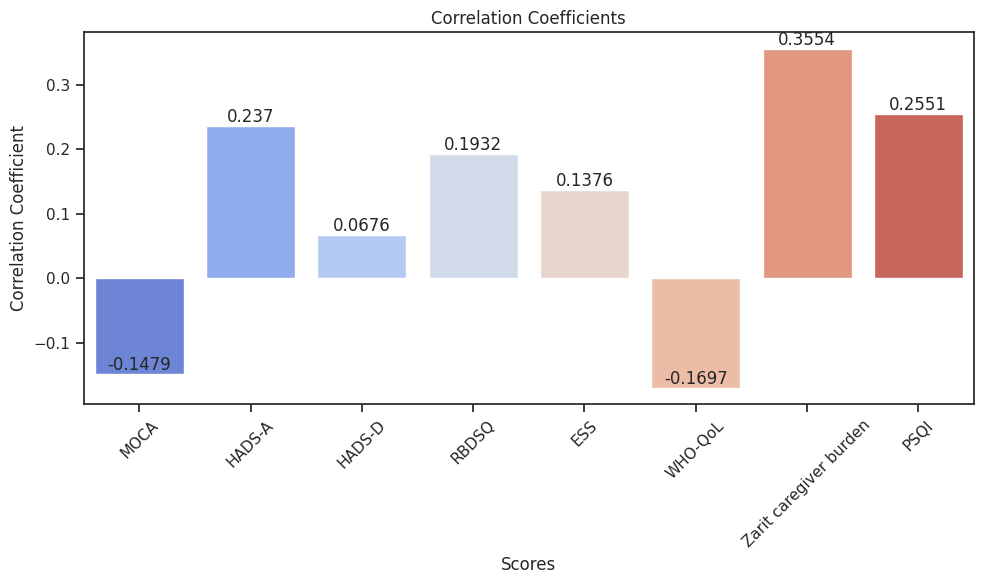
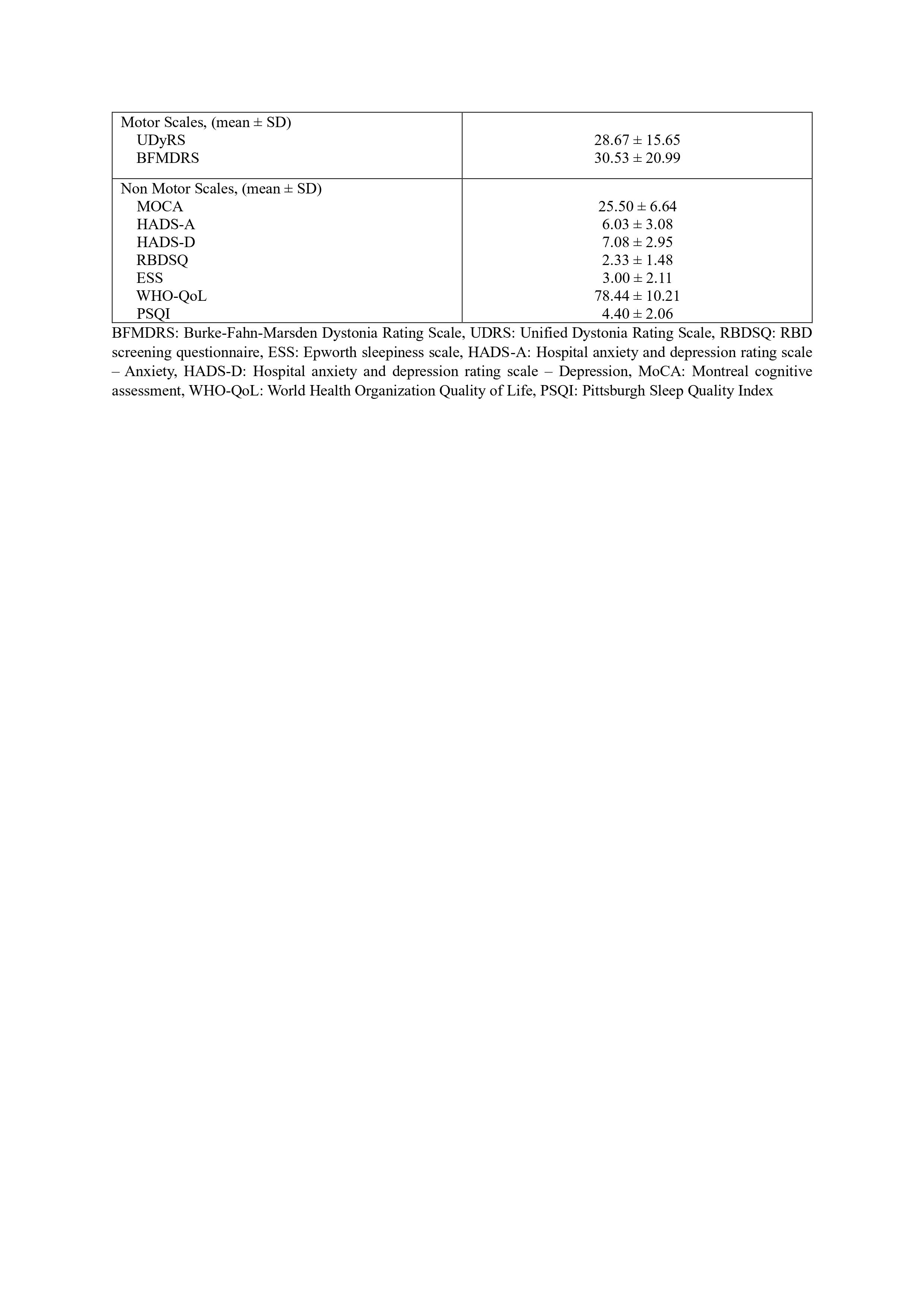
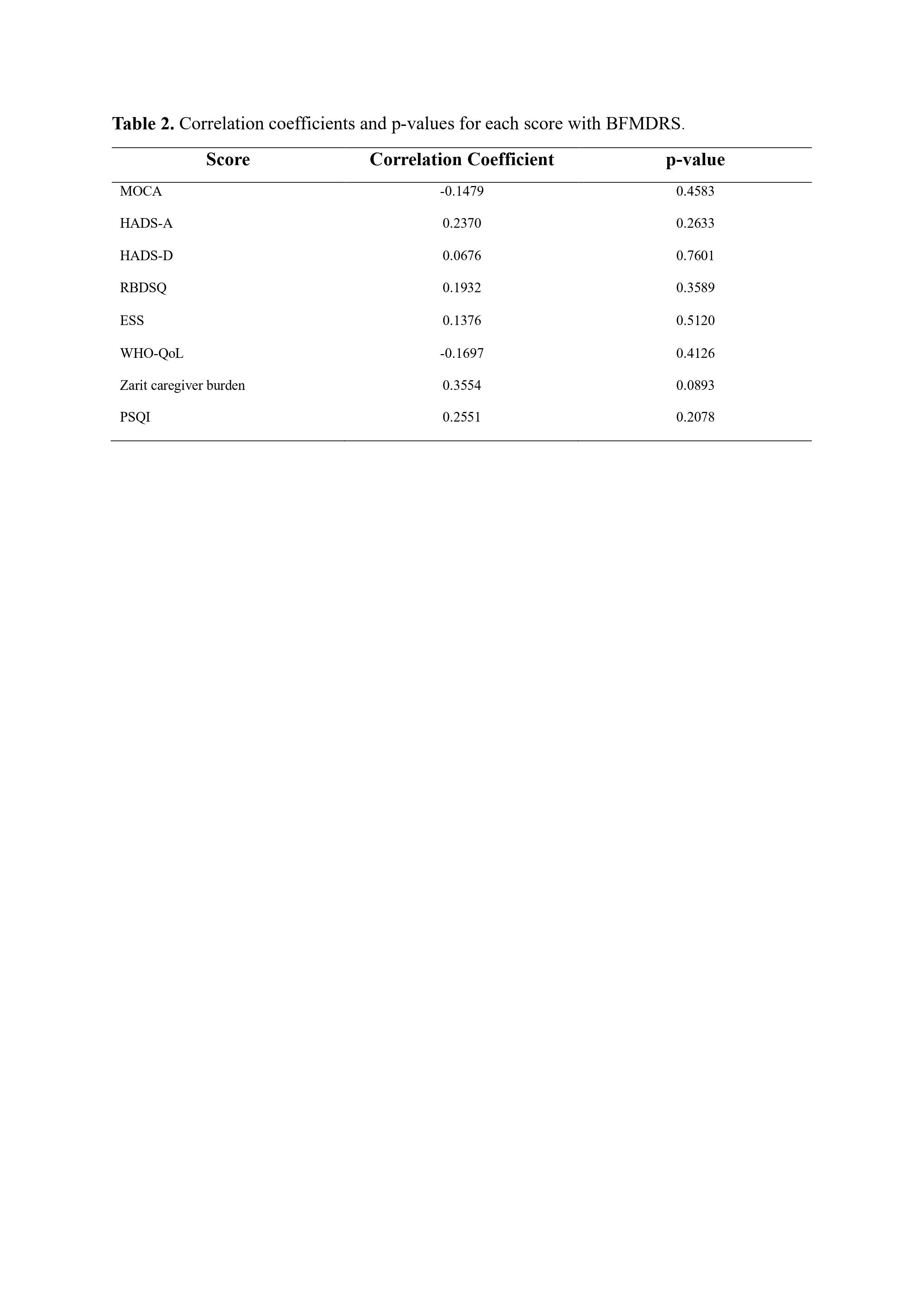
Results: The mean age was 28.63±11.96 years. Men (n=41) outnumbered women (n=19). The mean age of men (30.5±11.9 years) was higher than women (26.3 ± 8.5 years), but not significant (P=0.24). The mean age at disease onset was 21.01±13.89 years. Mean disease duration was 8.55±7.45 years. Subjectively the most common non-motor symptoms reported were pain, anxiety, reduced sleep and depression. Geste occurred in 29 patients without age, onset, or dystonia severity correlation. Generalized dystonia prevailed in infancy/childhood onset; segmental/multifocal dystonia in adolescence/adulthood onset. Other movement disorders (chorea, parkinsonism, myoclonus, ataxia) coexisted in 30%. Levodopa responded in 26.6% (16 patients). UDRS: 28.67±15.65, BFMDRS: 30.53±20.99. The mean MoCA score was 25.50±6.64. RBD was not observed in any of the patients with a mean RBDSQ score of 2.33±1.48. The ESS score was 3.00±2.11. The WHO-QoL score was 78.44±10.21. The HADS-A score was 6.03±3.08 and HADS-D score was 7.08±2.95. There was a positive correlation between BFMDRS score and the Zarit caregiver burden score that was not significant (p=0.089).
Conclusion: Our study provides a detailed account of various non-motor symptoms idiopathic dystonia. Dystonia severity correlates positively with caregiver burden, emphasizing holistic care. Non-significant correlations with specific non-motor symptoms underscore dystonia’s diverse impact. Results stress the necessity of comprehensive patient care and exploration of environmental-genetic factors in dystonia and non-motor symptoms’ etiology.
Fig 1 Non motor symptoms
Fig 3 Correlation coefficients and p-values
Table 1. Demographic and clinical characteristics.
Table 1. Demographic and clinical characteristics.
Table 2. Correlation coefficients and p-values
To cite this abstract in AMA style:
N. Gowda, N. Kamble, VV. Holla, R. Yadav, B. Muthusamy, PK. Pal. A Comprehensive Evaluation of the Non-Motor Symptoms, Quality of Life and Caregiver Burden in Patients with Idiopathic Dystonia [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/a-comprehensive-evaluation-of-the-non-motor-symptoms-quality-of-life-and-caregiver-burden-in-patients-with-idiopathic-dystonia/. Accessed July 13, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-comprehensive-evaluation-of-the-non-motor-symptoms-quality-of-life-and-caregiver-burden-in-patients-with-idiopathic-dystonia/