Category: Myoclonus
Objective: This article reviews the diagnosis, management, and prognosis of acute Post Hypoxic Myoclonus (PHM) with myoclonic status (MS) and status epilepticus (SE) based on a case.
Background: After cardiorespiratory arrest (CRA), neurologists are often consulted for determination of prognosis. One particularly important finding is acute PHM, which has been associated with poor outcome [1]. SE which presents concomitantly may also be an important factor in determining the outcome.
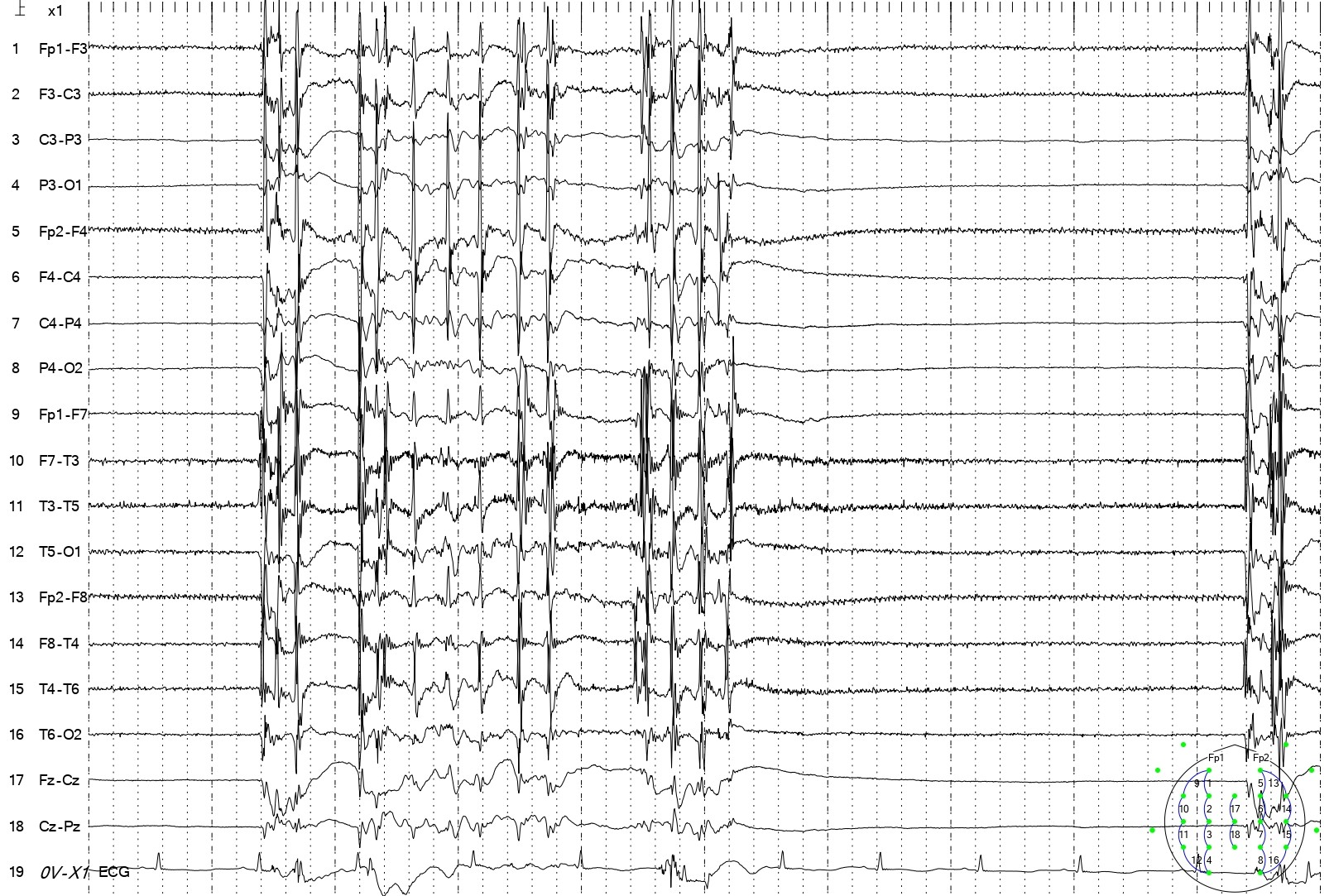
Method: A 79-year-old female with no history of movement disorder or seizure was consulted for periodic jerking movements on facial muscles and extremities. The movements began soon after the patient regained spontaneous circulation after resuscitation of CRA and was placed in mechanical ventilation. No improvement was seen with intravenous phenytoin 100 mg tid. She had a history of thyroid cancer, had undergone thyroidectomy and tracheostomy 2 weeks before. The contrast-enhanced brain computed tomography showed no lesion. The electroencephalogram (EEG) showed constant periodic general spikes and waves suggesting SE. Levetiracetam loading dose of 3000 mg via feeding tube, followed by 500 mg bid, resolved the movement. Subsequent EEG confirmed no epileptiform discharge. The patient eventually died after 2 weeks of treatment.
Results: Acute PHM is clinically defined by focal, multifocal, or generalized myoclonic movements of the face, trunk, extremities, and sternocleidomastoid and trapezius muscles that begin within 72 hours of cardiorespiratory arrest [1]. The patient was diagnosed with acute PHM, as the myoclonic jerks began no more than 24 hours after resuscitation. As valproic acid and levetiracetam are two most-used medications for PHM [2], levetiracetam was administered in the case and ceased SE. While MS is conventionally considered as an indicator of severe neurological injury and bad prognosis, this is challenged by increasing reports of cases with a favorable outcome [1]. It has been suggested that MS and SE are two different entities and must be separated when addressing the prognosis [3]. However, MS with concomitant SE made up a very poor survival rate [3].
Conclusion: The case showed that acute PHM was diagnosed mainly on clinical findings. The most important ancillary examination for PHM is the EEG, to determine any SE. Levetiracetam may control the MS and SE, but both conditions concomitantly make up a poor survival rate.
EEG showed periodic general spikes and waves.
References: 1. Freund B, Kaplan PW. Myoclonus After Cardiac Arrest: Where Do We Go From Here? Epilepsy Currents 2017; 17(5): 265-272.
2. Asghar A, Barnes B, Abdurahma A, Khan S, Primera G, Ravikumar N. Post hypoxic myoclonus: A tale of two minds. Epilepsy & Behavior Reports 2023; 21: 100589. https://doi.org/10.1016/j.ebr.2023.100589.
3. Brøchner AC, Lindholm P, Jensen MJ, Toft P, Henriksen FL, Lassen JF, Mikkelsen S. Post-Hypoxic Myoclonus Status following Out-of-Hospital Cardiac Arrest—Does It still Predict a Poor Outcome? A Retrospective Study. Healthcare 2022, 10, 41. https://doi.org/10.3390/healthcare10010041.
To cite this abstract in AMA style:
A. Kurniadi. A Poor Prognosis for Acute Post Hypoxic Myoclonus with Status Epilepticus: A Case Report [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/a-poor-prognosis-for-acute-post-hypoxic-myoclonus-with-status-epilepticus-a-case-report/. Accessed July 13, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-poor-prognosis-for-acute-post-hypoxic-myoclonus-with-status-epilepticus-a-case-report/