Category: Parkinsonism, Others
Objective: This project aims to address potential gaps in rural healthcare by assessing the feasibility of using mobile phone data to identify features of parkinsonism in a rural patient population in Gujarat, India.
Background: In many underserved areas of the world, there is a scarcity of neurologists. In low-income countries, there are around 0.03 per 100K neurologists, whereas there are 3 per 100K in high-income countries. As a result of this scarcity, the role of providing specialist care often will fall onto primary care physicians who are already overburdened in these underserved areas. For conditions such as Parkinson’s Disease (PD) or Essential Tremor (ET), proper and early diagnosis is important for long-term management. Yet, due to the lack of specialist availability and high burden on primary care physicians, there exists a gap in the detection and diagnosis of parkinsonism in rural patient populations.
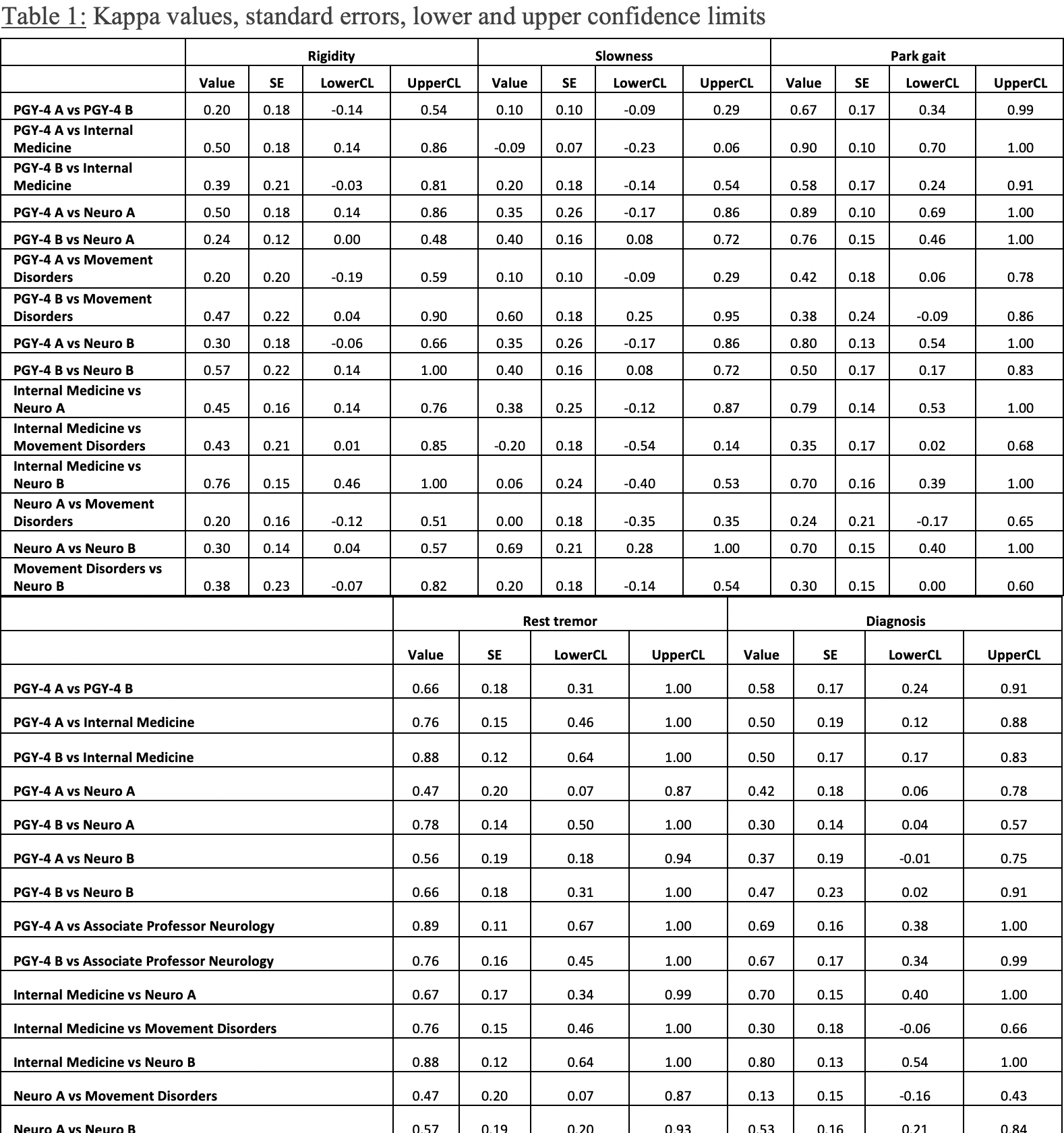
Method: In a pilot study, we collected data from a random sampling of patients from a rural area of Gujarat, India where patients were examined using a modified UPDRS scale. In this study, we developed a survey where clinicians indicated if features of parkinsonism (gait abnormality, slowness, rigidity, resting tremor) were present in each patient and whether they could diagnose parkinsonism. The raters consisted of 2 neurology resident PGY-4’s, 1 internal medicine attending, 2 neurology attendings, and 1 movement disorders specialist. Agreement and kappa statistics were calculated between different rater pairs.
Results: Notably, the kappa value for diagnosing parkinsonism between the internal medicine attending and the neurology attending was 0.7 and between the internal medicine attending and movement disorder attending was 0.8, showing substantial agreement. Furthermore, the levels of agreement between internal medicine attendings and neurology attendings for presence of gait abnormalities and tremor also was within the range of kappa values showing substantial agreement.
Conclusion: In underserved areas, it is often primary care physicians providing specialty care for patients. When using videos of patients examined through the UPDRS, internal medicine attendings diagnose parkonsinism with comparable reliability as movement disorder specialists. This suggests that, in areas with limited access to specialty care, mobile technology can be leveraged to diagnose patients early and provide expedited and efficient treatment.
Table 1
References: Berkowitz, A. L. (2014). Neurology education in resource-limited settings. Neurology.
Pagan, F. L. (2012). Improving Outcomes Through Early Diagnosis of Parkinson’s Disease. American Journal of Managed Care.
Tariq, Q. (2018). Mobile detection of autism through machine learning on home video: A development and prospective validation study. PLOS Medicine.
McHugh, M. (2012). Interrater reliability: the kappa statistic. Biochem Med (Zaghreb).
To cite this abstract in AMA style:
Z. Ahmed, S. Desai, A. Deb, S. Roy, D. Desai. Assessing Feasibility of Using Phone Video Data in Diagnosing Parkinsonism [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/assessing-feasibility-of-using-phone-video-data-in-diagnosing-parkinsonism/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/assessing-feasibility-of-using-phone-video-data-in-diagnosing-parkinsonism/