Objective: To identify potential risk factors for cortical Lewy Bodies (CLB) in the oldest-old (> 90 years old), we investigated if cardiovascular medical histories, medication use, or concurrent cerebrovascular neuropathological changes were associated with a higher likelihood of cortical Lewy Bodies (CLB) on autopsy.
Background: In younger ages (mean age 76 years), cerebrovascular lesions are associated with a higher likelihood of Parkinson’s and Alzheimer’s diseases, but a lower likelihood of Dementia with Lewy Bodies (Braak stage >4) [1]. However, the oldest-old frequently have multiple neurodegenerative processes occurring simultaneously [2].
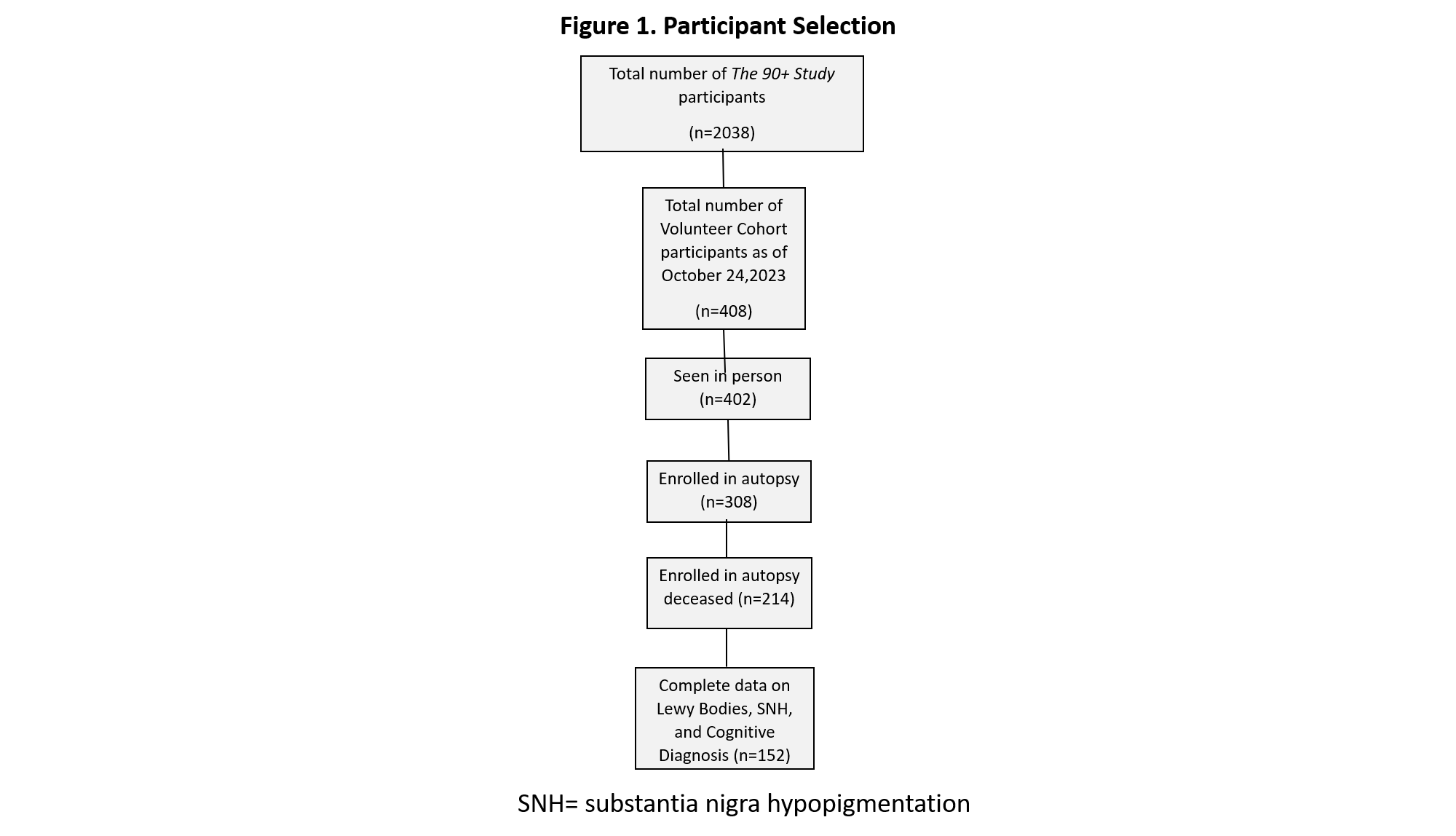
Method: Participants were from The 90+ Study, a prospective study of ageing and dementia in those aged > 90-years-old who completed questionnaires about their medical histories and medication use, and underwent autopsy (figure 1). We analyzed the volunteer subset who were not part of the Leisure World Cohort Study [3], as they represent a contemporary population assessed with the National Alzheimer’s Coordinating Center (NACC) Neuropathology form 10 or higher. CLB were considered present for a Braak stage > 4. We calculated odds ratios for the presence of CLB in relation to medical histories reported at last visit and medication use at any time using logistic regression models adjusted for age, sex, education, and the presence of other neuropathological changes. Chi-square tests for independence were used to determine the co-occurrence of CLB with cerebrovascular neuropathological changes. A complete list of the medical histories, medication classes, and neuropathological changes examined is provided in supplemental figure 1.
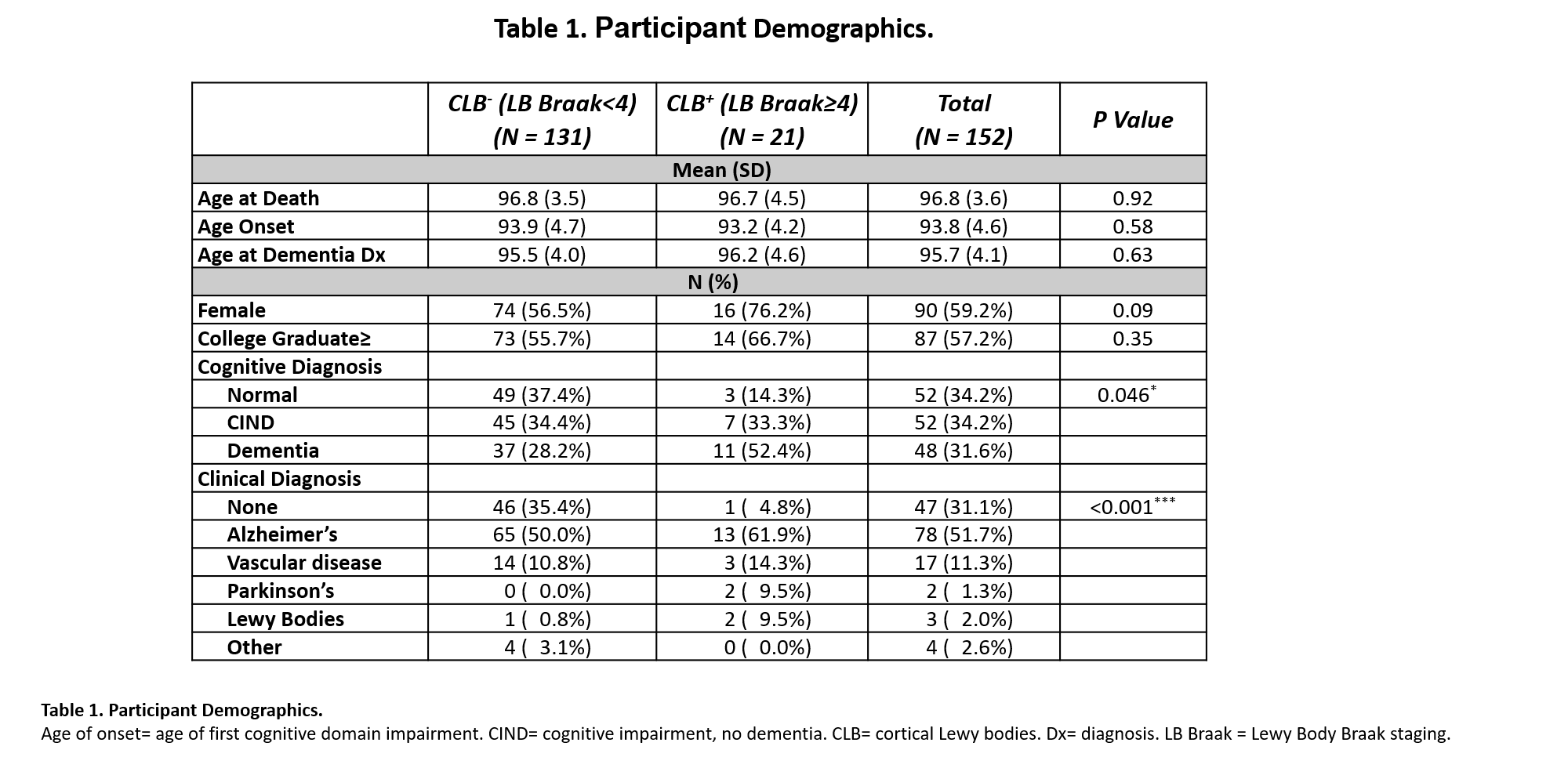
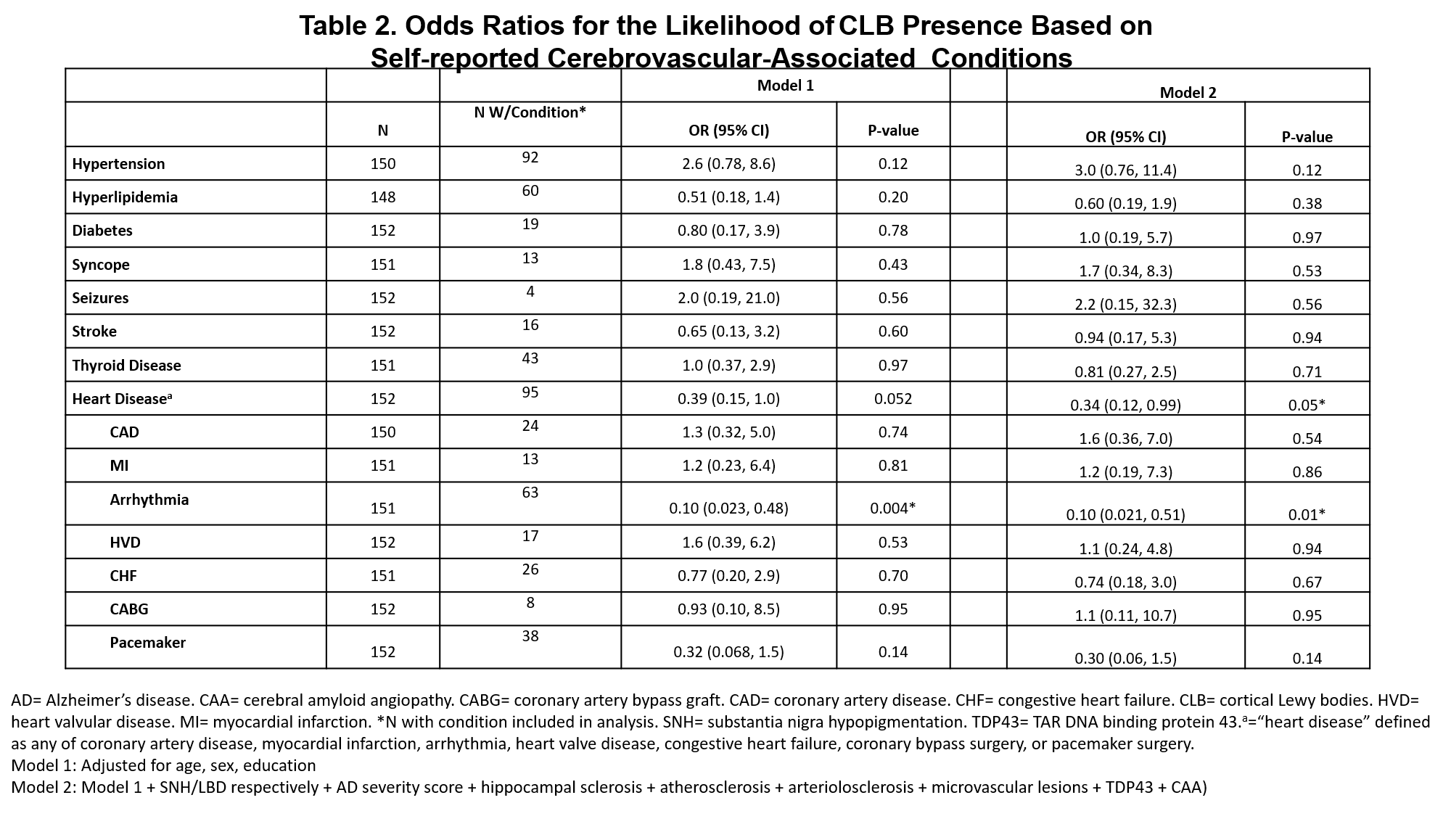
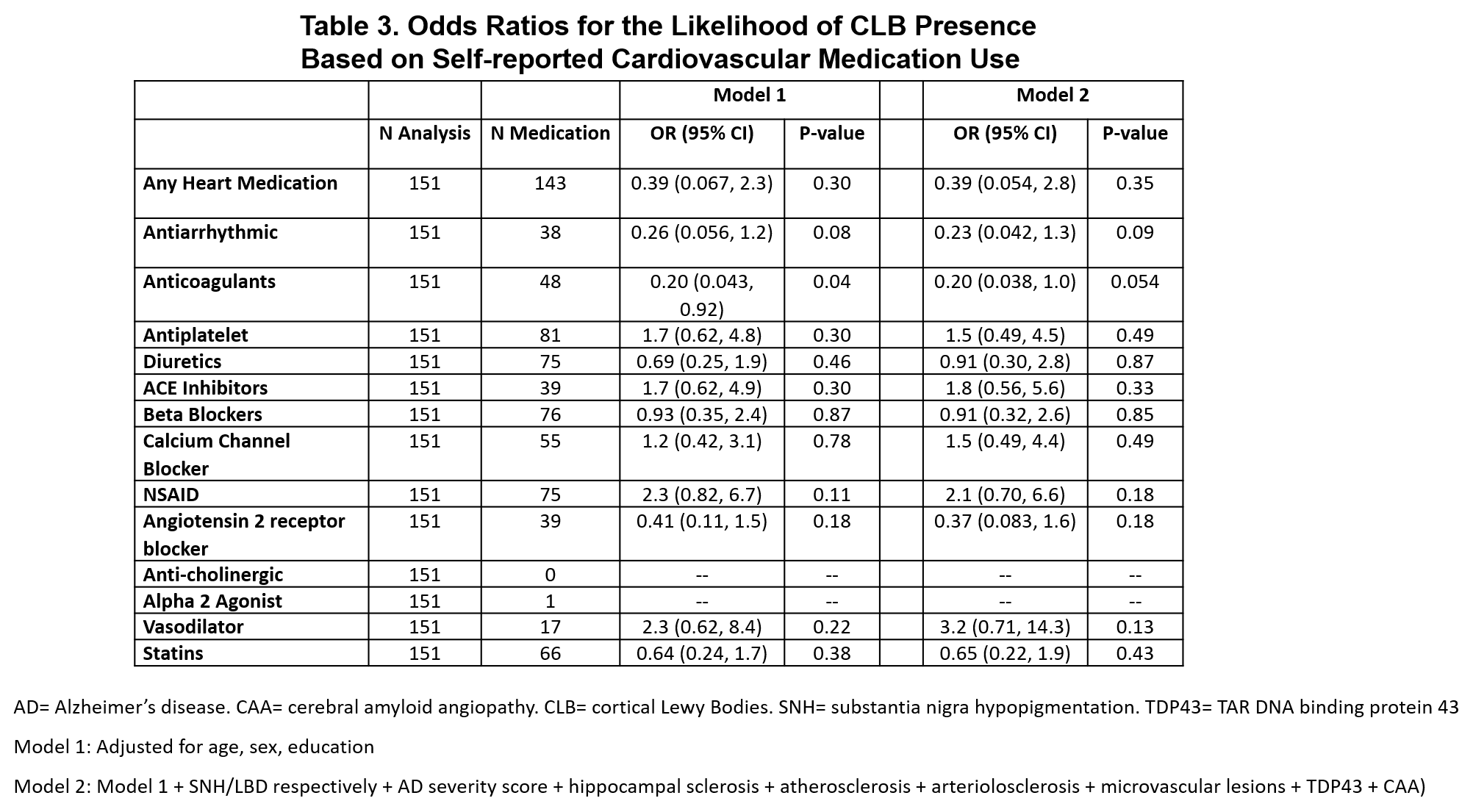
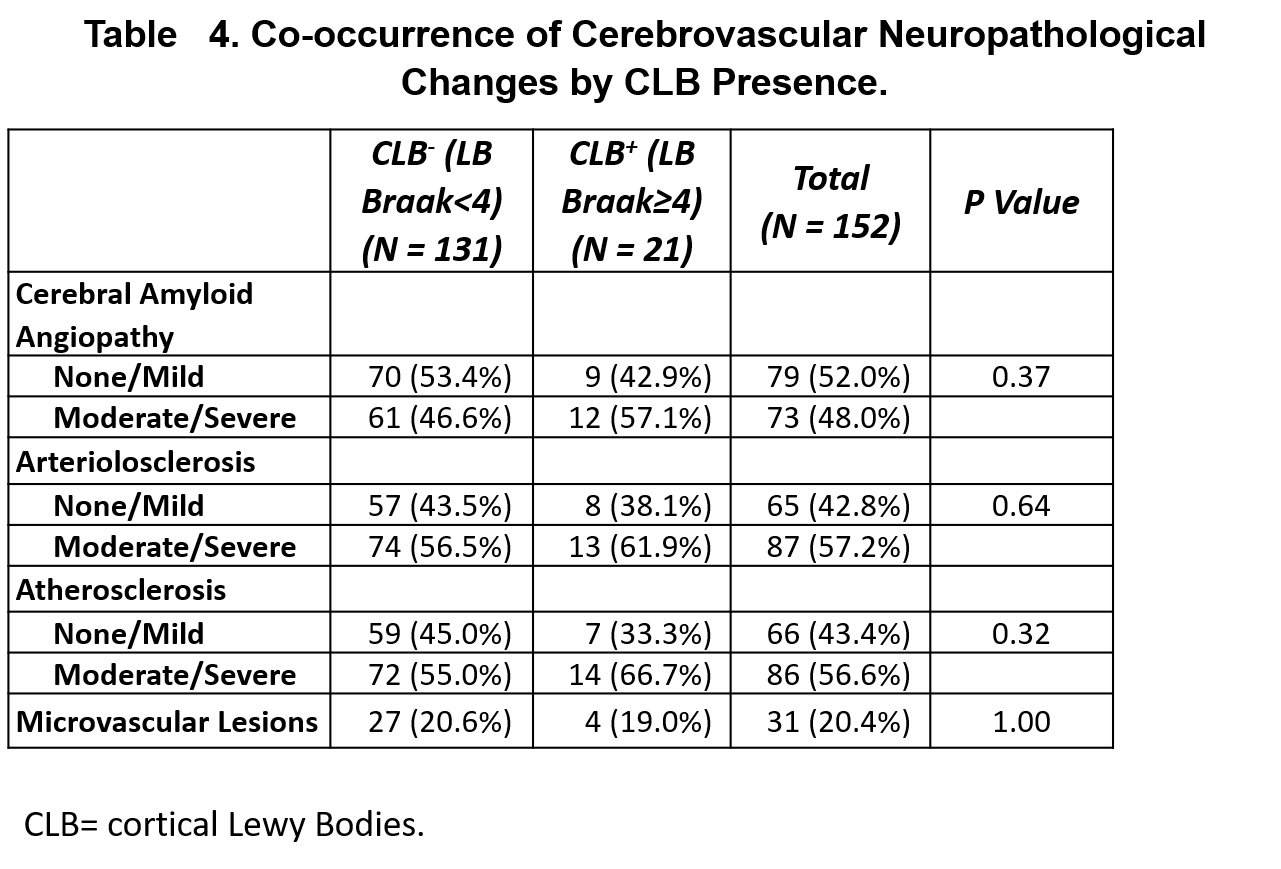
Results: For 152 participants, the mean age was 97, 59% were female, 57% were at least college educated, and 14% (n=21) had CLB (table 1). Arrythmia was associated with a lower likelihood of CLB presence (OR=0.10, 0.02-0.51) (table 2). Antiarrhythmics (0.23, 0.04-1.3) and anticoagulants (ACs) (0.20, 0.04-1.0) trended towards a lower likelihood of CLB (table 3). Cerebrovascular neuropathological changes were not associated with CLB presence (table 4).
Conclusion: The lower likelihood of CLB in participants with arrythmia may reflect benefit from medications rather than the condition itself. Further investigation into antiarrhythmics and ACs may clarify their potential as protective agents against CLB.
Figure 1
Table 1
Table 2
Table 3
Table 4
Supplemental figure 1
References: 1. Jellinger KA. Prevalence of vascular lesions in dementia with Lewy bodies. A postmortem study. J Neural Transm (Vienna). 2003;110(7):771-778. doi:10.1007/s00702-003-0824-x
2. Kawas CH, Kim RC, Sonnen JA, Bullain SS, Trieu T, Corrada MM. Multiple pathologies are common and related to dementia in the oldest-old: The 90+ Study. Neurology. 2015;85(6):535-542. doi:10.1212/WNL.0000000000001831
3. Melikyan ZA, Greenia DE, Corrada MM, Hester MM, Kawas CH, Grill JD. Recruiting the Oldest-old for Clinical Research. Alzheimer Dis Assoc Disord. 2019;33(2):160-162. doi:10.1097/WAD.0000000000000260
To cite this abstract in AMA style:
R. Rajmohan, Z. Al-Darsani, N. Phielipp, T. Montine, M. Corrada, C. Kawas. Cardiovascular Associations of Cortical Lewy Bodies in the Oldest Old: The 90+ study [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/cardiovascular-associations-of-cortical-lewy-bodies-in-the-oldest-old-the-90-study/. Accessed July 13, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/cardiovascular-associations-of-cortical-lewy-bodies-in-the-oldest-old-the-90-study/