Category: Parkinson's Disease: Neuroimaging
Objective: To investigate the impact of LRRK2 mutation in Parkinson disease (PD) and to explore the preclinical markers of LRRK2 mutation carriers who will develop PD.
Background: LRRK2 mutation is the most significant genetic risk factor for developing late-onset PD, accounting for around 1% of sporadic PD (sPD) and 4-36% of familial PD.1-3 To deepen our understanding of the mechanisms of LRRK2-related PD, we examined the clinical and brain morphological characteristics of non-manifest LRRK2 mutation carriers (LRRK2-NMC) and LRRK2-associated PD (LRRK2-PD) at the early stage.
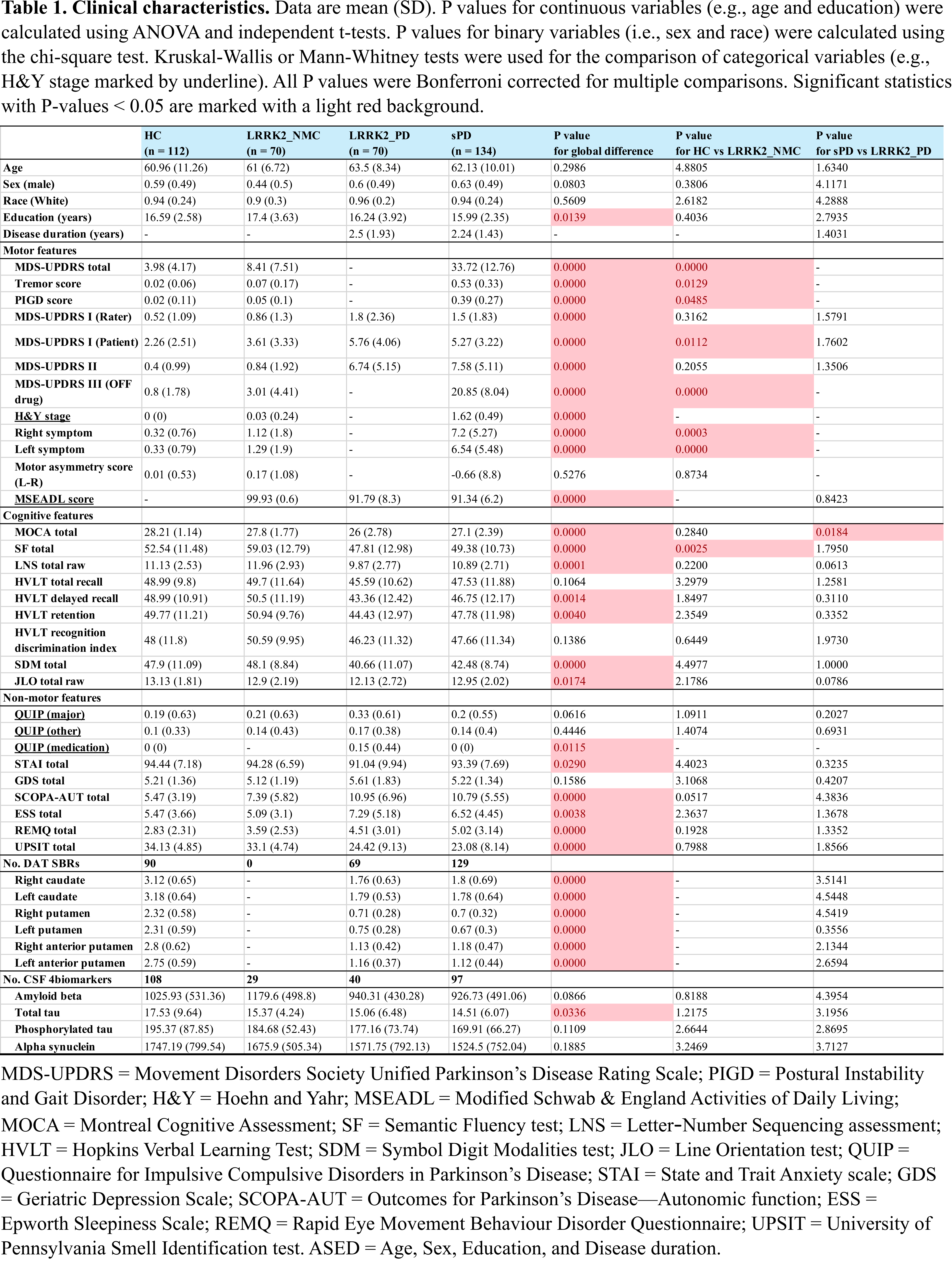
Method: We collected samples from the Parkinson’s Progression Marker Initiative (PPMI, www.ppmi-info.org/) and analyzed the clinical and T1 MRI data from 134 sPD, 70 LRRK2-PD, 70 LRRK2-NMC, and 112 healthy controls (HC).4The LRRK2 patients do not have known GBA variants associated with PD. All groups were matched for age and sex. LRRK2-PD and sPD groups were also matched for disease duration. The analyzed clinical characteristics include 1) demographic, cognitive, motor, and nonmotor features; 2) dopamine transporter binding ratio of bilateral caudate and putamen (DAT SBR); and 3) four PD-related CSF biomarkers. Brain morphological features include cortical thickness, surface area, and cortical volume (using FreeSurfer 7.2).
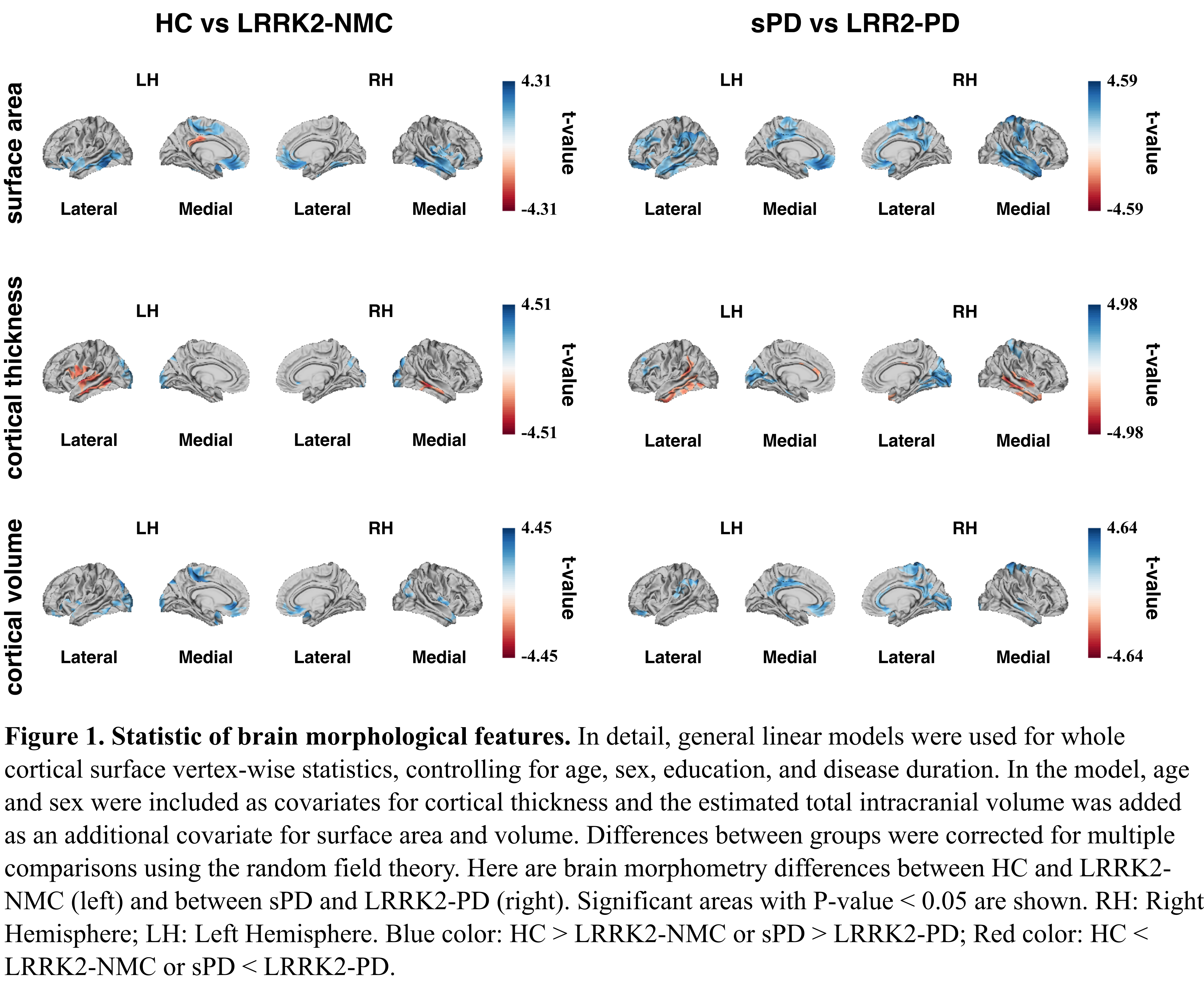
Results: Clinical and brain morphological characteristics of different groups are presented in Table 1 and Figure 1. In brief, the LRRK2-NMC group showed significantly higher MDS-UPDRS scores than HC, suggesting that LRRK2-NMC may already present slight motor deficits. Regions in the left paracentral lobe and prefrontal lobe showed lower surface area and cortical volume in LRRK2-NMC than in HC. Moreover, the MOCA score was lower in LRRK2-PD than in sPD, suggesting the severe cognitive decline in LRRK2-PD at the early disease stage. In terms of brain morphometry, LRRK2-PD patients showed smaller surface area and cortical volume in parts of the right paracentral lobe compared to sPD.
Conclusion: This study investigated the clinical and brain morphological characteristics of LRRK2 mutation carriers with and without PD, showing that early LRRK2-NMC presents different clinical and brain structural patterns compared to HC. Submitted on behalf of the PPMI LRRK2 analysis working group.
table 1.
figure 1.
References: 1. Tolosa E, Vila M, Klein C, Rascol O. LRRK2 in Parkinson disease: challenges of clinical trials. Nature Reviews Neurology 2020;16(2):97-107.
2. Taymans J-M, Fell M, Greenamyre T, et al. Perspective on the current state of the LRRK2 field. npj Parkinson’s Disease 2023;9(1).
3. Healy DG, Falchi M, O’Sullivan SS, et al. Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: a case-control study. The Lancet Neurology 2008;7(7):583-590.
4. Marek K, Jennings D, Lasch S, et al. The Parkinson progression marker initiative (PPMI). Progress in neurobiology 2011;95(4):629-635.
5. Worsley KJ, Marrett S, Neelin P, Vandal AC, Friston KJ, Evans AC. A unified statistical approach for determining significant signals in images of cerebral activation. Human Brain Mapping 1996;4(1):58-73.
To cite this abstract in AMA style:
Q. Tao, S. Rahayel, C. Tremblay, A. Vo, A. Dagher. Clinical and Brain Morphological Characteristics of Early LRRK2-associated Parkinson Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-and-brain-morphological-characteristics-of-early-lrrk2-associated-parkinson-disease/. Accessed July 15, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-and-brain-morphological-characteristics-of-early-lrrk2-associated-parkinson-disease/