Category: Drug-Induced Movement Disorders
Objective: To share an exciting case of a young lady with disabling generalized Tardive Dystonia (TD) with complete resolution of symptoms following bilateral Globus pallidus internus Deep Brain Stimulation (Gpi-DBS).
Background: Dystonia is the third most common movement disorder and is sometimes classified based on etiology [1]. One such etiology, TD occurs in the setting of neuroleptic medication usage and can be refractory to withholding the offending drug. For these patients, DBS can be considered as a potential therapy [2]. A recent meta-analysis demonstrated a substantial 67% improvement in the Burke‐Fahn‐Marsden Dystonia Rating Scale (BFMDRS) with the application of DBS in a cohort of these patients [3]. Here, we present a case of chronic disabling tardive dystonia that achieved near-complete resolution after bilateral GpiDBS.
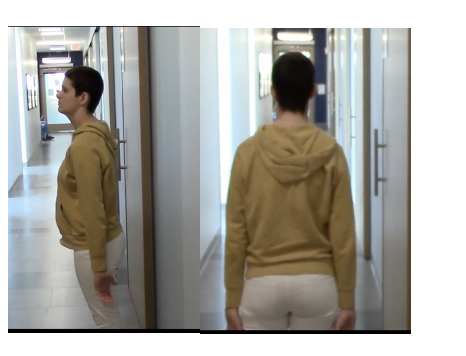
Method: A case report of 28-year-old woman with a history of bipolar disorder and prolonged use of neuroleptic medications (lithium, aripiprazole, paliperidone) presented with a 4-year progression of involuntary movements, causing pain and hindering mobility and daily activities. Neurological examination revealed thin muscle bulk, increased muscle tone, rigidity (predominantly in the upper extremities), dystonic movements of the head and neck with retrocollis and truncal extension, and an abnormal gait characterized by arching of the head, neck, and trunk [Figure 1]. Brain MRI was negative and genetic testing for dystonia was unremarkable.
Results: The patient was diagnosed with generalized tardive dystonia attributed to paliperidone, given the patient’s prolonged exposure to this medication for 1-2 years before the onset of symptoms. Conservative management was attempted with discontinuation of the implicated agents, as well as trials with Levodopa, Tetrabenazine, Trihexyphenidyl, amantadine, baclofen, and botox, however, the patient’s condition persisted. Subsequently, the patient underwent bilateral GpiDBS, resulting in a nearly complete resolution of symptoms [Figure 2]. Notably, the observed improvement has remained at the patients’ 4-year follow up.
Conclusion: Bilateral GPi-DBS was able to achieve symptomatic remission in a patient with generalized TD resistant to medical interventions. This case highlights the need to consider DBS placement in refractory TD in carefully selected patients, focusing on factors that could have contributed to a positive outcome.
Figure 1. Before DBS
Figure 2. After DBS
References: [1] The Dystonias – PMC [Internet]. [cited 2023 Sep 15]. Available from: https://www-ncbi-nlm-nih-gov.ezp.slu.edu/pmc/articles/PMC10226676/
[2] Factor SA. Management of Tardive Syndrome: Medications and Surgical Treatments. Neurotherapeutics. 2020 Oct;17(4):1694–712.
[3] Grabel M, Merola A. Pallidal deep brain stimulation for tardive dystonia: meta-analysis of clinical outcomes. Neurol Sci. 2023 Mar;44(3):827–33.
To cite this abstract in AMA style:
L. Okar, P. Murin, C. Pratap. Complete Resolution of Tardive Dystonia After Bilateral Globus Pallidus Interna Deep Brain Stimulation [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/complete-resolution-of-tardive-dystonia-after-bilateral-globus-pallidus-interna-deep-brain-stimulation/. Accessed June 30, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/complete-resolution-of-tardive-dystonia-after-bilateral-globus-pallidus-interna-deep-brain-stimulation/