Category: Myoclonus
Objective: To correlate local filed potential (LFP) spectral data with clinical improvement of the Unified Myoclonus Rating Scale (UMRS) in post-hypoxic myoclonus (PHM) syndrome treated with deep brain stimulation (DBS).
Background: We present a 56year old patient (pt) who suffered anoxic brain injury secondary to suicide attempt. Subsequently, the pt developed generalized seizures, with rest and action myoclonic jerks affecting all extremities. The pt was wheelchair bound and treatment was refractory to multiple medications. As a result, the pt was implanted with bilateral Globus Pallidus (GPi) DBS.
Method: LFP survey was conducted bilaterally for each available DBS contact following IPG implantation, showing high spectral power at 10-12 and 25Hz. Chronic recording was initiated post implantation at 10Hz to allow the clinician to observe changes in LFP activity until initial programming four weeks later. LFP streaming was performed during each clinic visit. These recordings were analyzed at 11Hz (highest spectral power) and 50Hz (gamma LFP to assess overall broadband activity) by counting LFP peaks that crossed frequency threshold. UMRS were analyzed at pre-DBS, 1, 3, and 6 months post-DBS and were correlated with LFPs.
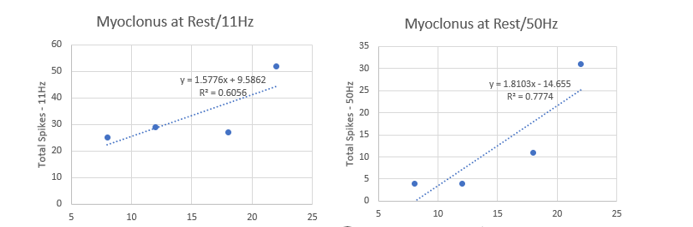
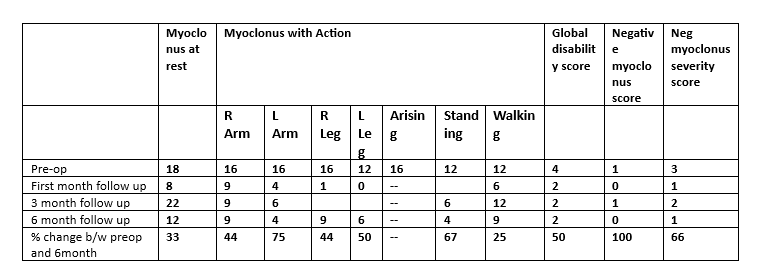
Results: The highest observed LFP activity was used to determine initial contact selection (contact 2 and 9). Myoclonus at Rest section of the UMRS were highly correlated to LFP activity at 11Hz and 50Hz (Pearson r=0.778 and 0.882, respectively [Figure1]. Over the course of 6 months, patient showed marked improvement in myoclonic jerks at rest, with further reduction in action and negative myoclonus. Patient was able to walk with the help of one person assistance and eat without assistance. At 6 months post DBS, pt showed 33% improvement in the myoclonus at rest, and 50% improvement in the global disability score based on the UMRS [Table1].
Conclusion: Our case demonstrates improvement in UMRS with bilateral GPi-DBS in a patient with PHM. Changes in rest myoclonus highly correlated with LFP suppression activity at both beta and gamma frequency peaks suggesting that LFP activity may help understand stimulation parameters and may provide insights into the disease.
Spike correlation with Myoclonus at rest 11-50Hz
Pre and post op assessment based on UMRS
References: 1. Ozturk G, Tasci I, Samanci MY, Peker S. Is deep brain stimulation useful in lance–adams syndrome? Neurology Asia. 2021;26(3):617-620.
http://dx.doi.org/10.54029/2021ykj
2. Asahi T, Kashiwazaki D, Dougu N, et al. Alleviation of myoclonus after bilateral pallidal deep brain stimulation for Lance-Adams syndrome. J Neurol. 2015;262(6):1581-1583.
http://dx.doi.org/10.1007/s00415-015-7748-x
3.Gao F, Ostrem JL, Wang DD. Treatment of Post-Hypoxic Myoclonus using Pallidal Deep Brain Stimulation Placed Using Interventional MRI Methods. Tremor Other Hyperkinet
Mov (N Y). 2020;10:42. http://dx.doi.org/10.5334/tohm.544
4. Kim MJ, Park SH, Heo K, Chang JW, Kim JI, Chang WS. Functional Neural Changes after Low-Frequency Bilateral Globus Pallidus Internus Deep Brain Stimulation for Post-Hypoxic Cortical Myoclonus: Voxel-Based Subtraction Analysis of Serial Positron Emission. Brain Sci. 2020;10(10). http://dx.doi.org/10.3390/brainsci10100730
5.Mure H, Toyoda N, Morigaki R, Fujita K, Takagi Y. Clinical Outcome and Intraoperative Neurophysiology of the Lance-Adams Syndrome Treated with Bilateral Deep Brain
Stimulation of the Globus Pallidus Internus: A Case Report and Review of the Literature. Stereotact Funct Neurosurg. 2020;98(6):399-403. http://dx.doi.org/10.1159/000509318
6. Ramdhani RA, Frucht SJ, Kopell BH. Improvement of Post-hypoxic Myoclonus with Bilateral Pallidal Deep Brain Stimulation: A Case Report and Review of the Literature.
Tremor Other Hyperkinet Mov (N Y). 2017;7:461. http://dx.doi.org/10.7916/D8NZ8DXP
7. Yamada K, Sakurama T, Soyama N, Kuratsu J. Gpi pallidal stimulation for Lance-Adams syndrome. Neurology. 2011;76(14):1270-1272. http://dx.doi.org/10.1212/WNL.0b013e31821482f4
To cite this abstract in AMA style:
H. Kaur, T. Goble, A. Fenoy, R. Ramdhani. Deep Brain Stimulation for Post-Hypoxic Myoclonus: A Case Correlating Local Field Potentials to Clinical Outcome [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/deep-brain-stimulation-for-post-hypoxic-myoclonus-a-case-correlating-local-field-potentials-to-clinical-outcome/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/deep-brain-stimulation-for-post-hypoxic-myoclonus-a-case-correlating-local-field-potentials-to-clinical-outcome/