Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To identify speech biomarkers to assess impulsivity in patients with Parkinson’s disease (PwPD).
Background: Although PD mainly presents with motor symptoms, the burden of neuropsychiatric and behavioral manifestations, including depression, impulsivity, and apathy, greatly affects patients’ well-being, quality of life, and prognosis. Specifically, impulsive-compulsive disorders have been reported as side effects of dopaminergic medication [1] and may also arise during deep brain stimulation [2].
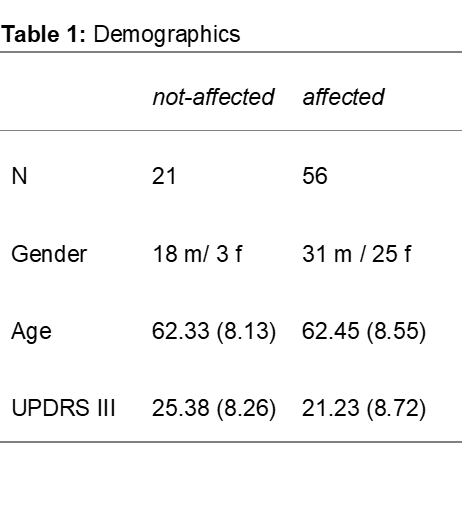
Method: 77 PwPD (aged 42 to 81) completed three speech tasks, i.e. rapid syllable repetition of /pa/-/ta/-/ka/ (DDK), reading (TXT), and rhythmic repetition of the syllable /pa/ (RHY), underwent a motor assessment (UPDRS III), and completed the “Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease Rating Scale” (QUIP-RS) [2]. PwPD were divided into two groups based on their QUIP scores (questions A to D, Table 1). Those with scores between 0 and 10 were deemed “not affected,” while those with scores of 11 or higher were deemed “affected.” Acoustic speech features were automatically extracted using the ki:elements speech processing engine SIGMA. These features were correlated with QUIP scores, adjusting for age, sex, and UPDRS III, using partial Spearman rank correlations. Furthermore, speech features were compared between the two clinical groups using an ANCOVA, adjusted for age, sex, and UPDRS.
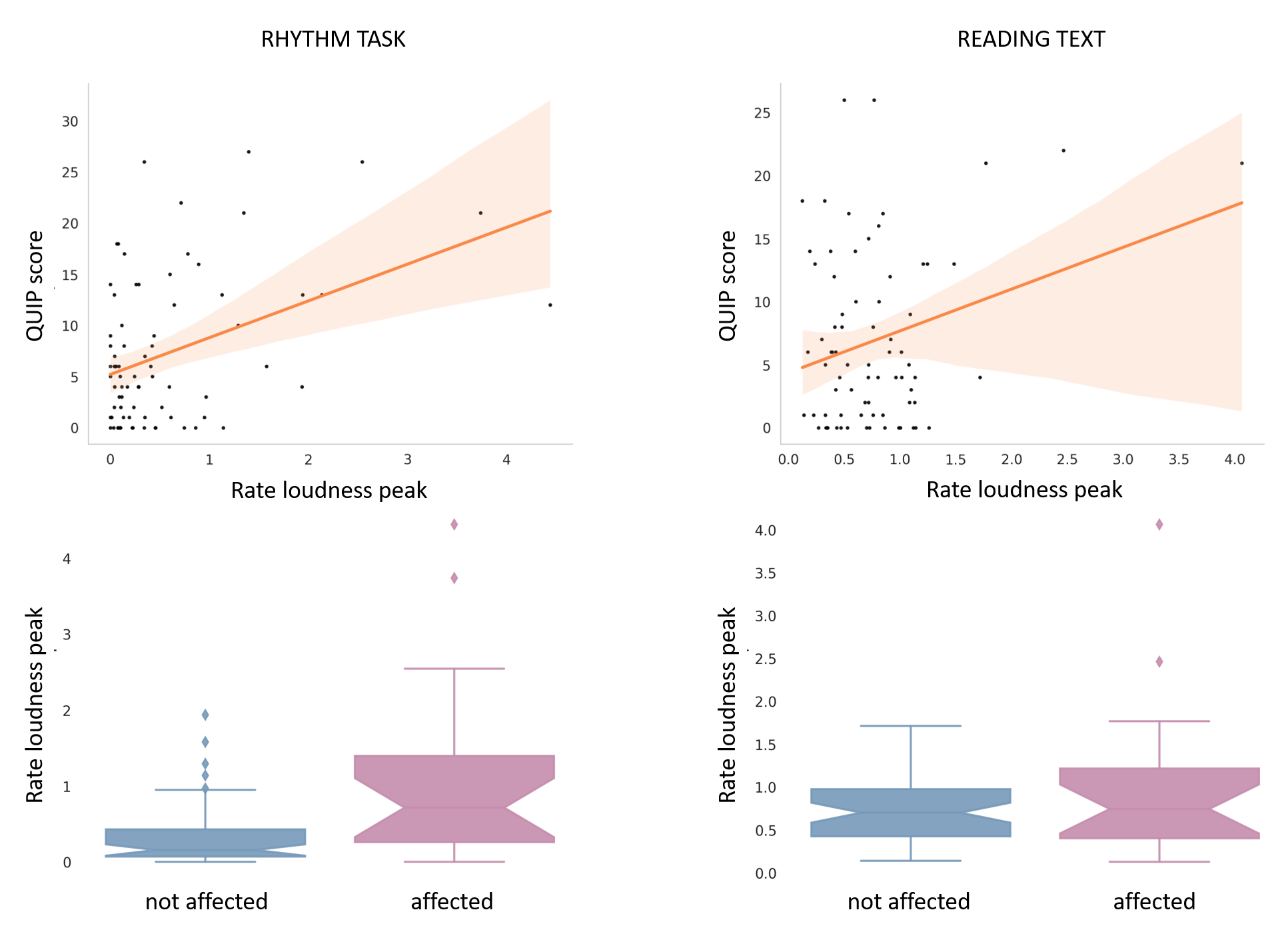
Results: Corrrelations showed an association between the QUIP score and the number of loudness peaks per second in both the rhythm (r = .41, p < 0.001) and the reading task (r = .32, p < .01). Additionally, both features differed significantly between the two groups (RHY: p < .001 | TEXT: p < .05, Figure 1).
Conclusion: Excessive loudness variation appears linked to impulsivity, with the effect being more pronounced in the rhythm task, indicating task specificity. This suggests that speech tasks play a crucial role. Given that precise control is affected in people with impulse control issues, this not only affects behaviors like eating or shopping but also speech. In summary, this proof-of-principle study highlights speech analysis as a powerful, non-invasive tool for identifying non-motor symptoms such as impulsivity in PD. While further validation and optimization are needed, integrating speech analysis into patient care could offer avenues for personalized interventions in the future.
Table 1
Figure 1
References: [1] Voon, V., Hassan, K., Zurowski, M., De Souza, M., Thomsen, T., Fox, S., … & Miyasaki, J. (2006). Prevalence of repetitive and reward-seeking behaviors in Parkinson disease. Neurology, 67(7), 1254-1257.
[2] Scherrer, S., Smith, A. H., Gowatsky, J., Palmese, C. A., Jimenez-Shahed, J., Kopell, B. H., … & Figee, M. (2020). Impulsivity and compulsivity after subthalamic deep brain stimulation for Parkinson’s disease. Frontiers in Behavioral Neuroscience, 14, 47.
[3] Probst, C. C., Winter, L. M., Möller, B., Weber, H., Weintraub, D., Witt, K., … & van Eimeren, T. (2014). Validation of the questionnaire for impulsive-compulsive disorders in Parkinson’s disease (QUIP) and the QUIP-rating scale in a German speaking sample. Journal of Neurology, 261, 936-942.
To cite this abstract in AMA style:
T. Thies, E. Mallick, S. Jost, J. Tröger, M. Barbe. Detecting impulsivity through speech in patients with Parkinson’s Disease: A principle proof study [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/detecting-impulsivity-through-speech-in-patients-with-parkinsons-disease-a-principle-proof-study/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/detecting-impulsivity-through-speech-in-patients-with-parkinsons-disease-a-principle-proof-study/