Category: Parkinsonism, Atypical: PSP, CBD
Objective: To retrospectively look at atypical Parkinsonism mimics in our cohort and reappraise the clinical features of these subset of patients
Background: Atypical parkinsonism syndromes (APS) include PSP (progressive supranuclear palsy), CBS (Corticobasal syndrome), MSA (Multiple system atrophy) and DLBD (Diffuse Lewy Body Disease). Many other conditions beyond sporadic neurodegeneration can mimic APS. These conditions are labelled as atypical atypical parkinsonism or atypical parkinsonism mimics. Identifying these patients is essential given the clinical, therapeutic and research implications
Method: Medical records of patients with a clinical diagnosis of atypical parkinsonism (AP) from January 2015 to November 2023 from the National Institute of Mental Health and Neurosciences- Movement Disorder database were reviewed retrospectively. AP patients having atypical features for diagnosis of PSP, CBD, and MSA were identified. Clinical data and investigations of these patients were collected and charted. Atypical features for PSP – Age< 40 years, Significant family history, Episodic memory, Hallucinations, autonomic failure, Multisegmented UMN and LMN signs, Appendicular Ataxia. For CBS- Significant family history, Logopenic and semantic primary progressive aphasia, Hallucinations, autonomic failure, cerebellar signs, Multisegmented UMN and LMN signs. For MSA- Age < 30 years, Significant family history, cognitive involvement, visual hallucination, dementia, down gaze palsy or slowing of vertical saccades
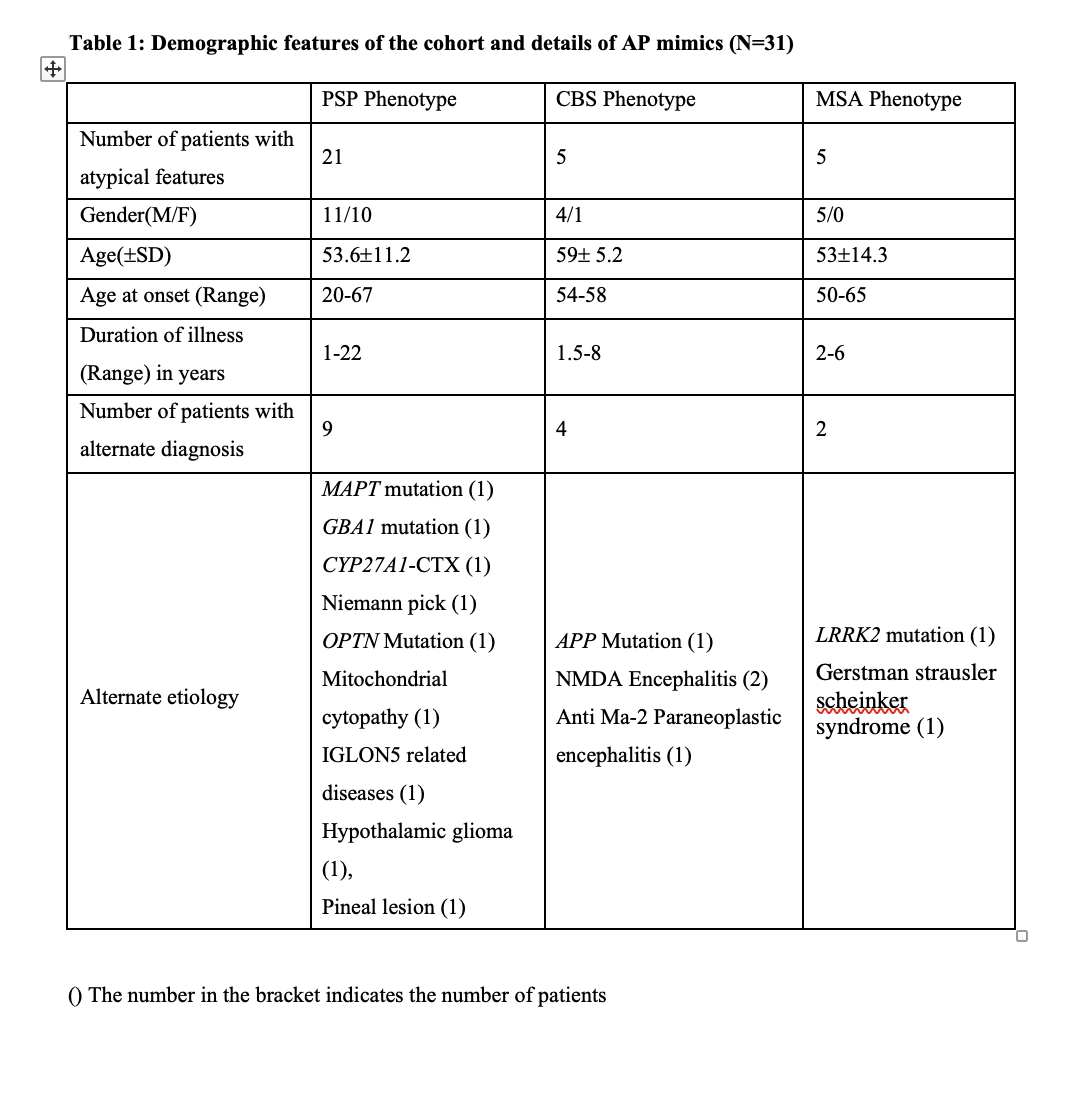
Results: 184 patients of atypical parkinsonism (PSP-86 MSA-61, CBS-37) were enrolled. Among these, 31 patients had atypical features for diagnosis of PSP, CBD, and MSA. 15 patients received alternate diagnosis after evaluation. Among PSP group, 21 patients had atypical features of which 9 patients received an alternate diagnosis. Among CBS group 5 patients had atypical features, 4 patients had an alternate diagnosis. In MSA group 5 patients had atypical features and 2 of them had an alternate diagnosis. Demographics features and etiology of atypical parkinsonism mimics were given in Table 1.
Conclusion: Our study shows that conditions beyond sporadic neurodegeneration can mimic APS. Among atypical parkinsonism mimics in our cohort, genetic conditions are most common. Young age of onset, rapid or slow progression, positive family history may be helpful to diagnose these AP mimics
Demographic features of the cohort and AP mimics
References: 1. Hirschbichler, S. T. et al. “Atypical” atypical parkinsonism: Critical appraisal of a cohort.
Parkinsonism Relat D 37, 36–42 (2017).
2. Höglinger, G. U. et al. Clinical diagnosis of progressive supranuclear palsy: The movement
disorder society criteria. Movement Disord 32, 853–864 (2017).
3. Armstrong, M. J. et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 80,
496–503 (2013).
4. Wenning, G. K. et al. The Movement Disorder Society Criteria for the Diagnosis of Multiple
System Atrophy. Mov. Disord. 37, 1131–1148 (2022).
5. Stamelou, M., Quinn, N. P. & Bhatia, K. P. “Atypical” atypical parkinsonism: New genetic
conditions presenting with features of progressive supranuclear palsy, corticobasal degeneration, or
multiple system atrophy—A diagnostic guide. Mov. Disord. 28, 1184–1199 (2013).
To cite this abstract in AMA style:
P. Katragadda, V. Holla, N. Kamble, R. Yadav, P. Pal. Diagnostic Spectrum in a Cohort of Atypical Atypical Parkinsonism [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/diagnostic-spectrum-in-a-cohort-of-atypical-atypical-parkinsonism/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/diagnostic-spectrum-in-a-cohort-of-atypical-atypical-parkinsonism/