Category: Parkinsonism, Others
Objective: Identify the predisposing or exacerbating factors of sleep disorders in Parkinson’s disease, and examine their association with levodopa treatment.
Background: Parkinson’s disease (PD) is a neurodegenerative condition marked by the depletion of dopaminergic neurons in the substantia nigra pars compacta. Although the initial treatment with carbidopa/levodopa effectively addresses motor symptoms, its prolonged administration can result in disturbances in the circadian rhythm. Additionally, Parkinson with patients (PwP) commonly encounter sleep disorders all of which notably diminish their quality of life.
Method: This observational, retrospective, single-center study analyzed the REMEPARK protocol database spanning from 2010 to 2024 were included, and a sample of 352 patients was obtained after applying inclusion and exclusion criteria. Demographic variables, clinical history, treatments, and scales such as UPDRS, NMS, and PDQ-8 were utilized. Fisher’s exact test was employed for categorical variables, while Mann-Whitney’s U test was used for numerical variables without a normal distribution. The Kolmogorov-Smirnov test confirmed the normal distribution of numerical values. Binary logistic regression, employing the backward stepwise method (AR) based on partial maximum likelihood estimates, was conducted to identify risk factors. Only variables significant in the univariate analysis and those deemed relevant to the model were included. All statistical analyses were carried out using the SPSS (IBM) statistical software.
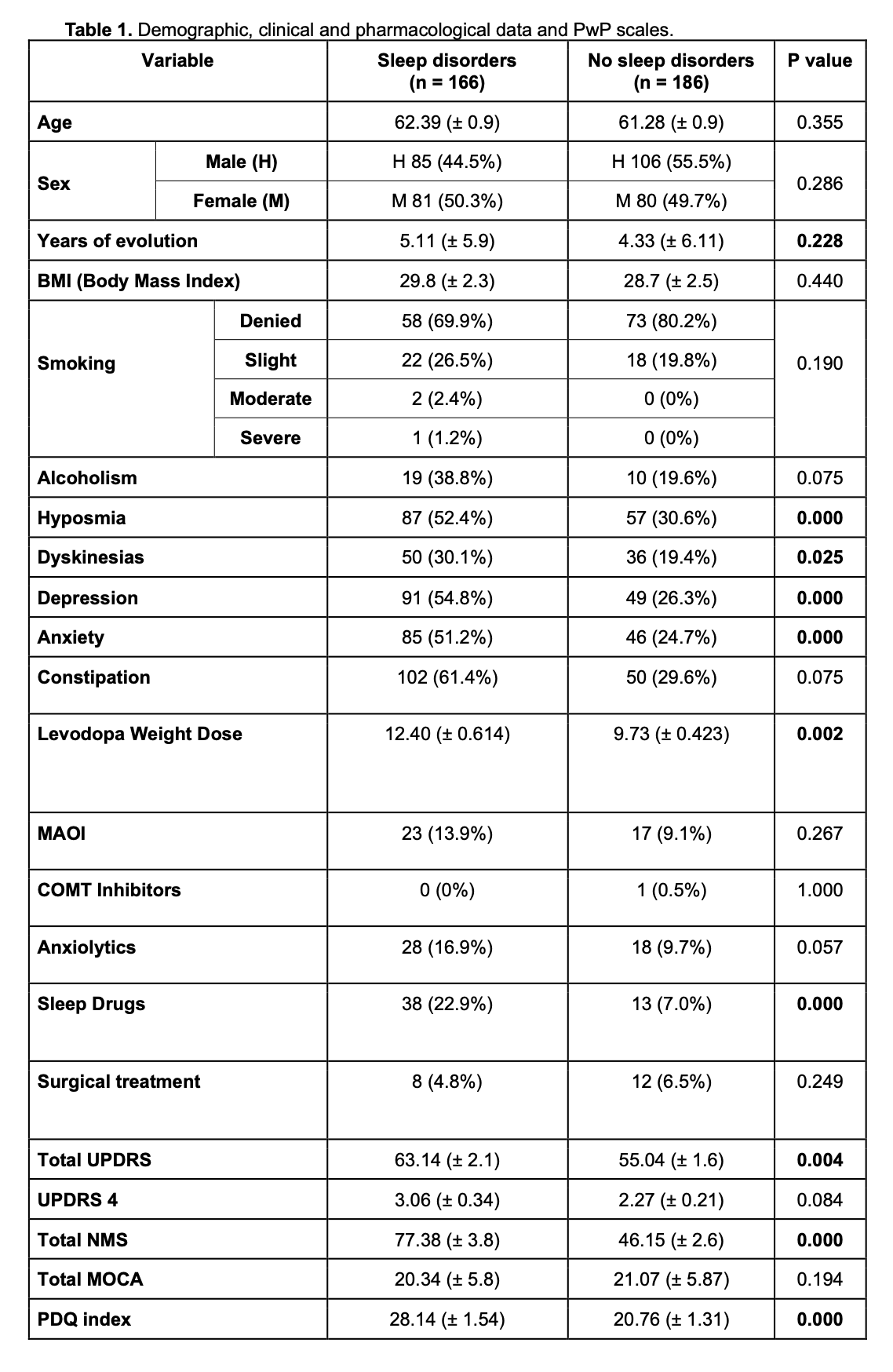
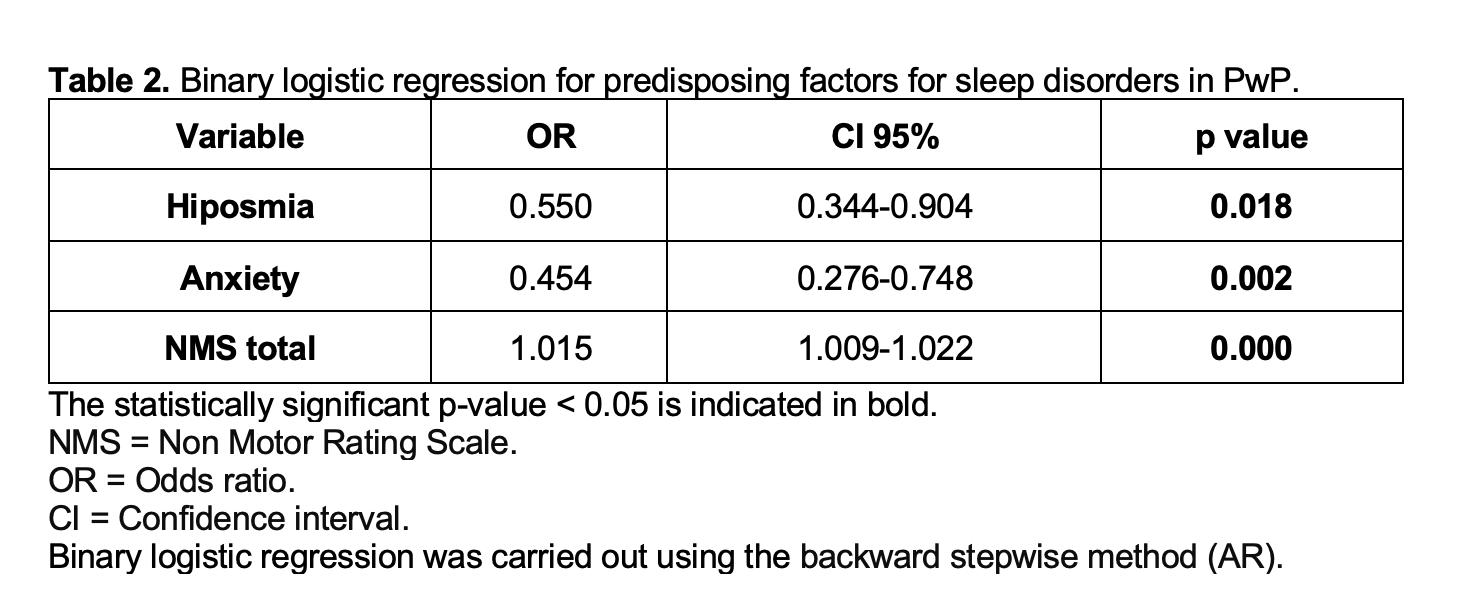
Results: A total of 352 PwP (54.2% males, 45.8% females, mean age 62.3 ±12.9 years) were recruited. Overall prevalence of sleep disturbances was 47.1% with 65.4% reporting insomnia, 33.3% reporting sleep behavioral disorder, and 1.2% reporting restless leg syndrome. Demographic, clinical, pharmacological backgrounds, and scale comparisons between groups are detailed in [Table1]. The binary logistic regression model design, controlled for age, disease duration, OFF time, MDS-UPDRS total score, PDQi, and levodopa weight dosage, is shown in [Table2].
Conclusion: Sleep disturbances are common non-motor manifestations in PD. Deliberately interviewing on risk factors may help to identify PwP at risk of sleep disorders to evaluate and treat them in a timely manner. Our regression model proved hyposmia, anxiety, and NMSS total score as independent risk factors for presenting a sleep disorder.
Table 1.
Table 2.
References: Parkinson J. An Essay on the Shaking Palsy. JNP. 2002;14:223–36. Disponible en: https://doi.org/10.1176/jnp.14.2.223.
Simon DK, Tanner CM, Brundin P. Parkinson Disease Epidemiology, Pathology, Genetics, and Pathophysiology. Clinics in Geriatric Medicine. 2020;36:1–12. Disponible en: https://doi.org/10.1016/j.cger.2019.08.002.
Halli-Tierney AD, Luker J, Carroll DG. Parkinson Disease. Am Fam Physician. 2020 Dec 1;102(11):679-691. PMID: 33252908.
Zuzuárregui JRP, During EH. Sleep Issues in Parkinson’s Disease and Their Management. Neurotherapeutics. 2020;17:1480–94. Disponible en: https://doi.org/10.1007/s13311-020-00938-y.
Stefani A, Högl B. Sleep in Parkinson ‘s disease. Neuropsychopharmacol. 2020;45:121–8. Disponible en: https://doi.org/10.1038/s41386-019-0448-y.
Hunt J, Coulson EJ, Rajnarayanan R, Oster H, Videnovic A, Rawashdeh O. Sleep and circadian rhythms in Parkinson’s disease and preclinical models. Mol Neurodegeneration. 2022;17:2. Disponible en: https://doi.org/10.1186/s13024-021-00504-w.
Taximaimaiti R, Luo X, Wang X-P. Pharmacological and Non-pharmacological Treatments of Sleep Disorders in Parkinson’s Disease. CN. 2021;19:2233–49. Disponible en: https://doi.org/10.2174/1570159X19666210517115706.
Picillo M, Phokaewvarangkul O, Poon Y, McIntyre CC, Beylergil SB, Munhoz RP, et al. Levodopa Versus Dopamine Agonist after Subthalamic Stimulation in Parkinson ‘s Disease. Movement Disorders. 2021;36:672–80. Disponible en: https://doi.org/10.1002/mds.28382.
Martínez-Ramírez D, Rodríguez-Violante M, Velázquez-Ávila ES, Cervantes-Arriaga A, González-Cantú A, Corona-Vázquez T, et al. Incidencia y distribución geográfica de la enfermedad de Parkinson en México. Salud Publica Mex. 2020;62:873–5. Disponible en: https://doi.org/10.21149/11750.
To cite this abstract in AMA style:
SF. Arechavala Lopez, I. Fuentes Calvo, AJ. Hernández-Medrano, A. Cervantes-Arriaga, M. Rodríguez-Violante. Exploring Retrospectively the Predisposing Factors of Sleep Disorders in Parkinson’s Disease. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/exploring-retrospectively-the-predisposing-factors-of-sleep-disorders-in-parkinsons-disease/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/exploring-retrospectively-the-predisposing-factors-of-sleep-disorders-in-parkinsons-disease/