Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To investigate the levels of fecal calprotectin (a marker of intestinal inflammation), in patients with Parkinson’s Disease (PD) and multiple system atrophy (MSA) compared to healthy controls.
Background: Recent studies suggest that intestinal dysbiosis and inflammation play a role in the patho-mechanims of neurodegenerative diseases. Previous studies reporting elevated fecal calprotectin in PD patients were limited by small sample size, and literature regarding intestinal inflammation in MSA remains scarce.
Method: We recruited 71 PD patients, 38 MSA patients and 60 age-matched healthy controls. Demographic data and clinical history were collected. PD and MSA severity was assessed using the MDS-UPDRS and UMSARS, respectively. Fecal metabolites were extracted and fecal calprotectin analyzed using enzyme-linked immunosorbent assay. All persons involved in the laboratory analyses were blinded to the subjects’ diagnosis and other clinical data.
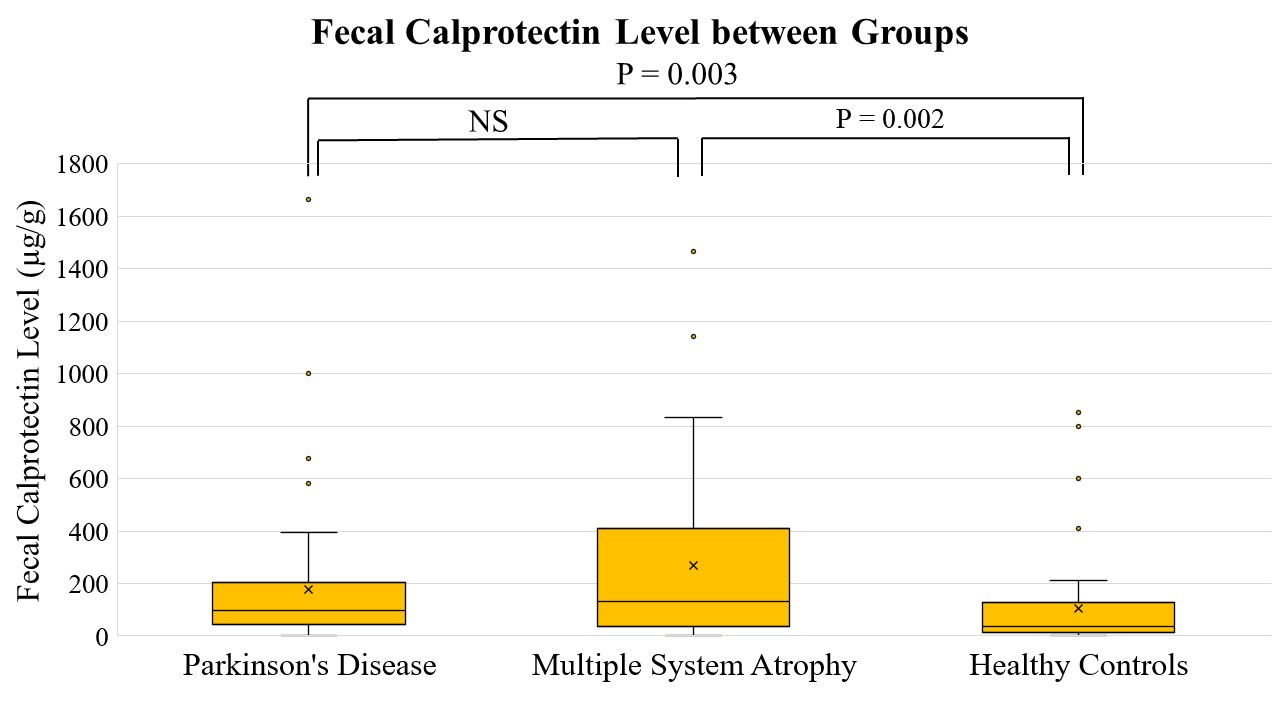
Results: Fecal calprotectin was significantly elevated in PD (176.5µg/g ± 174.2) and MSA patients (269.0µg/g ± 345.5) compared to healthy controls (106.0µg/g ± 174.2), but without significant difference between PD and MSA (Fig. 1). In the overall cohort, fecal calprotectin levels did not correlate with age, sex, smoking status, body mass index, and constipation severity. In the PD and MSA subgroups, fecal calprotectin did not correlate with disease duration, age of onset, and levodopa equivalent daily dosage. There were also no correlations with PD motor subtype (tremor dominant vs. postural instability-gait disorder), PD motor severity (MDS-UPDRS part III), severity of motor response complications (MDS-UPDRS part IV), MSA subtype (cerebellar- vs. parkinsonian-predominant), and MSA severity (total of UMSARS parts I and II).
Figure 1: Fecal calprotectin levels in Parkinson’s disease, multiple system atrophy and healthy controls. Comparison between groups was analyzed using Kruskal-Wallis Test. NS=Not significant.
Conclusion: PD and MSA patients had higher degrees of intestinal inflammation as evaluated by fecal calprotectin compared to controls. Calprotectin levels did not correlate with disease subtype or severity. Further studies are needed to understand the pathophysiology and impact of intestinal inflammation in these neurodegenerative disorders.
To cite this abstract in AMA style:
JW. Hor, ES. Khor, KK. Chong, SL. Song, CW. Chong, SY. Lim, AH. Tan. Fecal Calprotectin in Parkinson’s Disease and Multiple System Atrophy [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/fecal-calprotectin-in-parkinsons-disease-and-multiple-system-atrophy/. Accessed July 18, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/fecal-calprotectin-in-parkinsons-disease-and-multiple-system-atrophy/