Category: Technology
Objective: I) To compare digital mobility outcomes (DMOs) of free-living gait quality and quantity obtained over one week between people with Parkinson’s disease (PwPD) who experience freezing of gait (freezers) and those without (non-freezers). II) To assess if DMOs provide better biomarkers for freezer classification than clinical tests.
Background: Freezers typically walk slower with shorter steps and higher step-to-step variability than non-freezers when tested in the laboratory. It is still unknown if these deficits are worse during free-living gait and whether freezers have reduced everyday gait quantity.
Method: 531 PwPD from the Mobilise-D study were included and classified as freezers based on self-report (NFOG-Q>0). An array of DMO features were obtained from a lower-back wearable device and averaged over 7 consecutive days. Clinical gait tests included the Timed Up and go (TUG) and the 6 minute walk test ON medication. Independent T-tests compared freezers with non-freezers on demographics, clinical tests and average DMOs. ROC analysis AUC was applied to identify the best DMO biomarker and compare it to clinical tests.
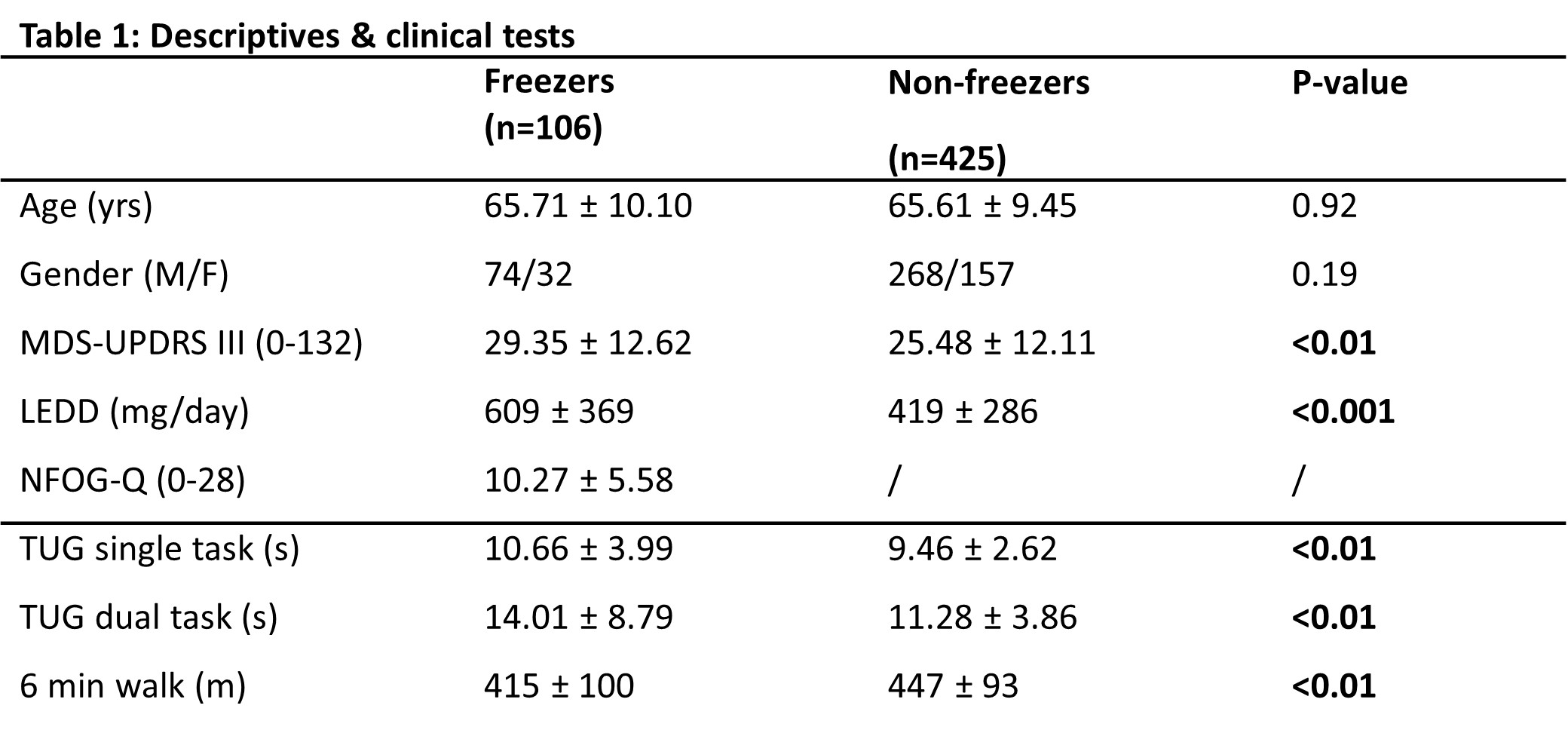
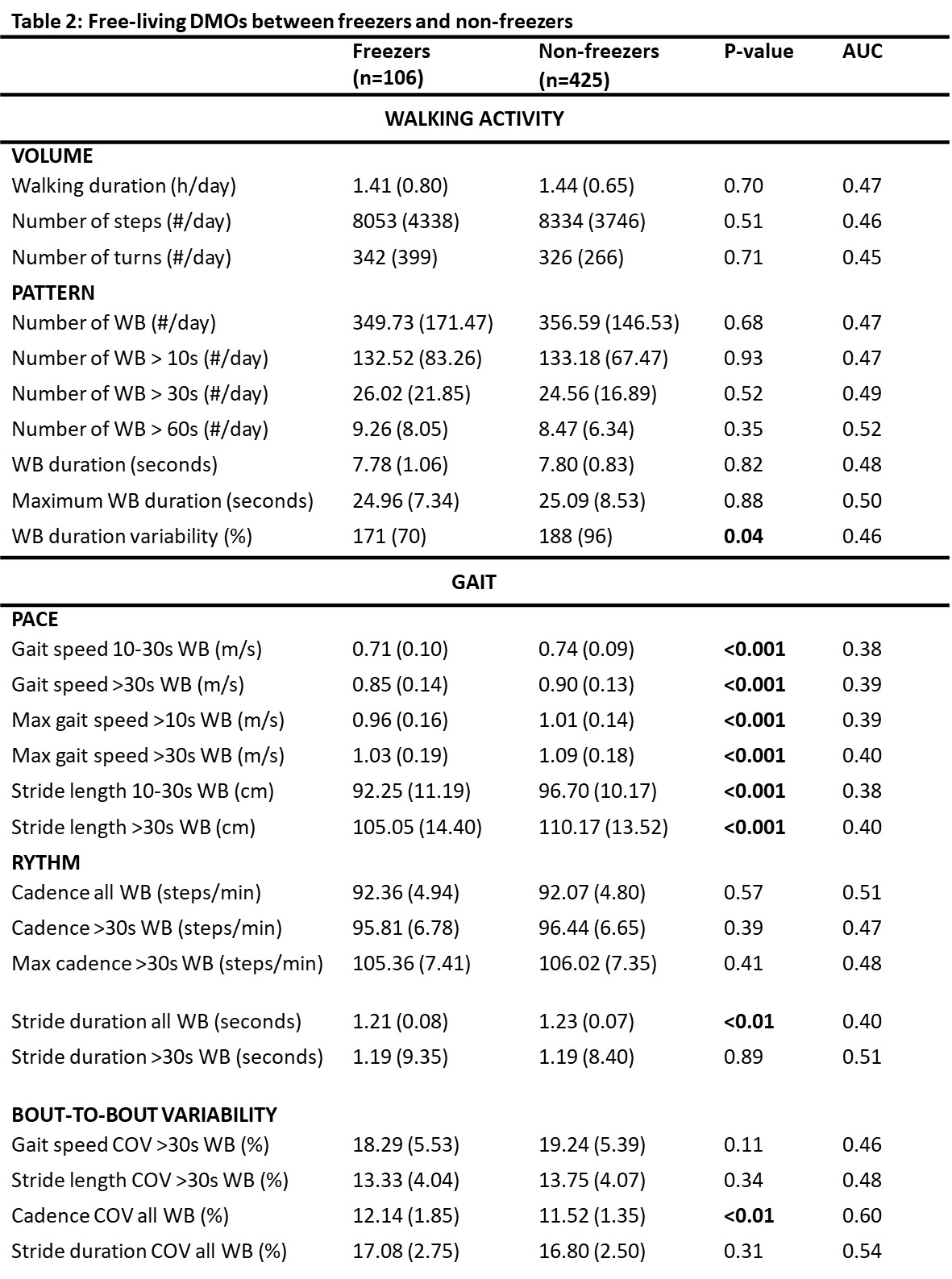
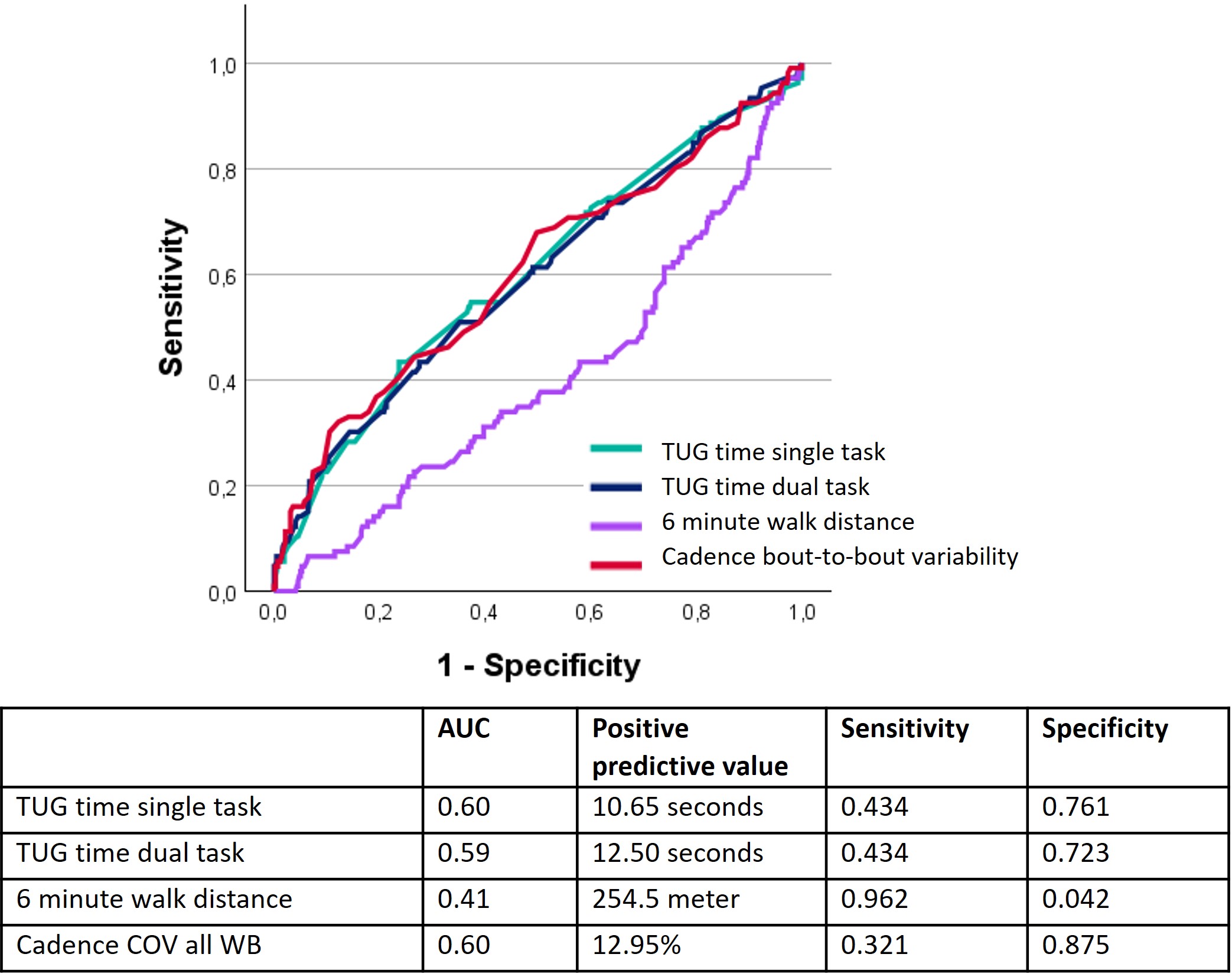
Results: 106 freezers and 425 non-freezers were identified. Groups had similar age and gender, but freezers had higher MDS-UPDRS III and LEDD scores [Table 1]. TUG and 6 minute walk test performance was better in non-freezers than freezers [Table 1]. In line with prior lab-based measurements, freezers took shorter strides and walked slower during daily-life [Table 2]. Surprisingly, walking quantity was similar between groups with a similar daily total walking duration, number of steps and number of turns. Of all DMO metrics, bout-to-bout variability in cadence was the best FOG biomarker with high specificity of 0.88 [Figure 1], albeit with poor sensitivity of 0.32 (AUC=0.6). This was comparable to the TUG time (AUC=0.6), which was the best clinical test FOG biomarker, but with a slightly higher sensitivity (0.43) yet reduced specificity (0.76).
Conclusion: As expected, freezers walked slower and with shorter strides during daily life, but they kept walking with the same quantity. Weekly-averaged DMOs only offer a suboptimal FOG biomarker. Further analysis on daily and even hourly data is warranted and likely to provide better biomarkers for FOG.
Table 1
Table 2
Figure 1
To cite this abstract in AMA style:
P. Ginis, E. Gazit, C. Schlenstedt, H. Gassner, C. Hansen, A. Mirelman, L. Alcock, C. Becker, J. Aymerich, L. Rivera, C. Kirk, H. Hunter, I. Neatrour, J. Kudelka, H. Hildesheim, P. Goerrissen, M. Gordon, L. Delgado, B. Caulfield, M. Long, M. Gilat, L. Rochester, A. Yarnall, W. Maetzler, J. Hausdorff, A. Nieuwboer. Free-living digital mobility outcomes in Parkinson’s disease patients with and without freezing of gait: what can they tell us? [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/free-living-digital-mobility-outcomes-in-parkinsons-disease-patients-with-and-without-freezing-of-gait-what-can-they-tell-us/. Accessed July 9, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/free-living-digital-mobility-outcomes-in-parkinsons-disease-patients-with-and-without-freezing-of-gait-what-can-they-tell-us/