Session Information
Date: Wednesday, September 25, 2019
Session Title: Cognition and Cognitive Disorders
Session Time: 1:15pm-2:45pm
Location: Agora 3 East, Level 3
Objective: The aim of this study was to compare the structure of gut microbiota and short-chain fatty acid(SCFAs) in PD with mild cognitive impairment (PD-MCI), PD with normal cognition (PD-NC) and healthy controls in southern China as well as to determine whether PD with cognitive declining is associated with alteration in the gut microbiome and its metabolite-SCFA.
Background: Mounting studies suggest that the altered gastrointestinal (GI) bacteria plays an important role in neurodegeneration disease, including Alzheimer’s disease(AD) and Parkinson’s disease(PD). However, the relationship between GI bacteria and PD with mild cognitive impairment remains unexplored.
Method: We analyzed fecal bacterial composition of 13 PD-MCIs, 14 PD-CNs and 13 healthy volunteers by using 16S rRNA next-generation-sequencing and Gas Chromatography-Mass Spectrometer(GC-MS).
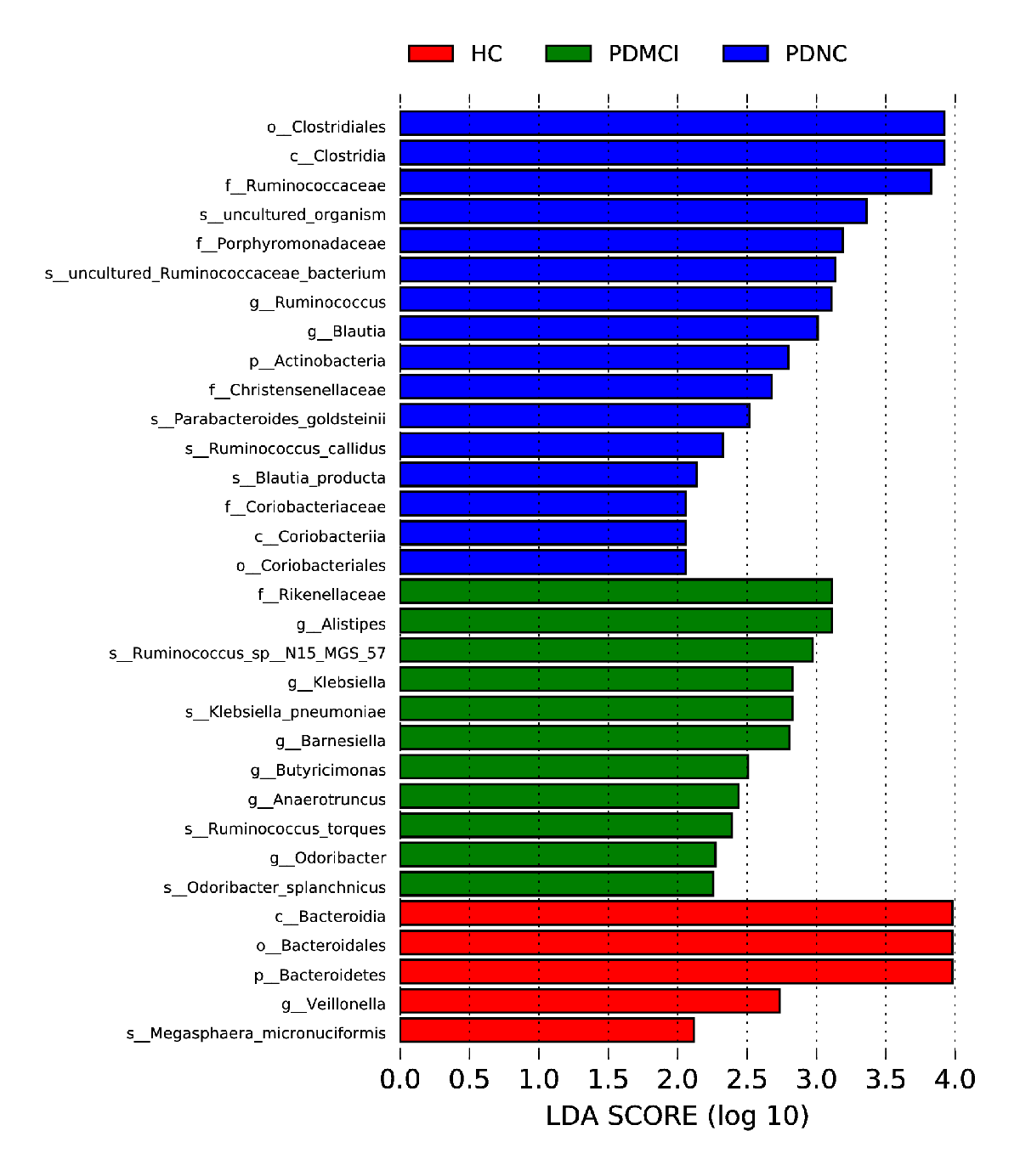
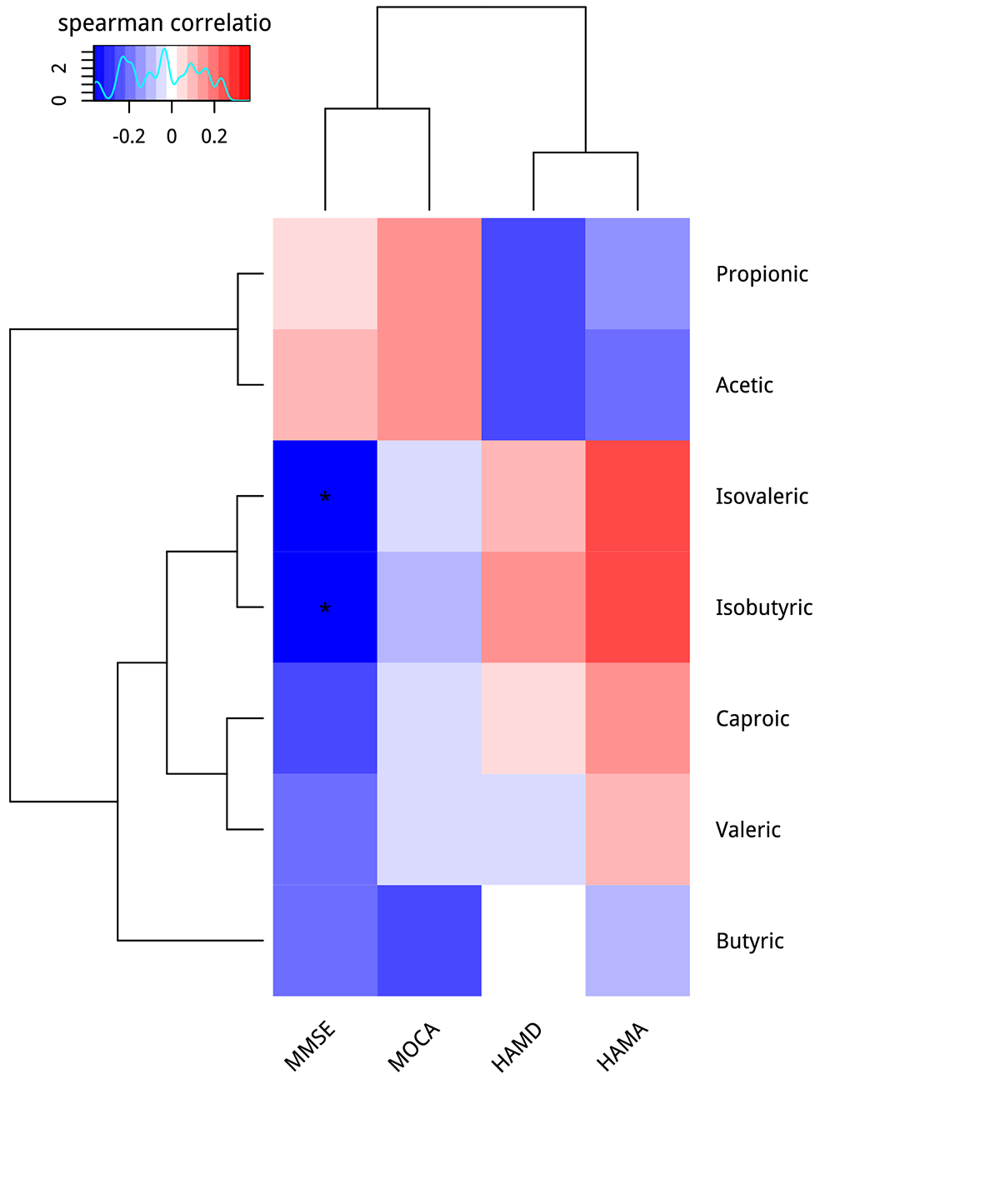
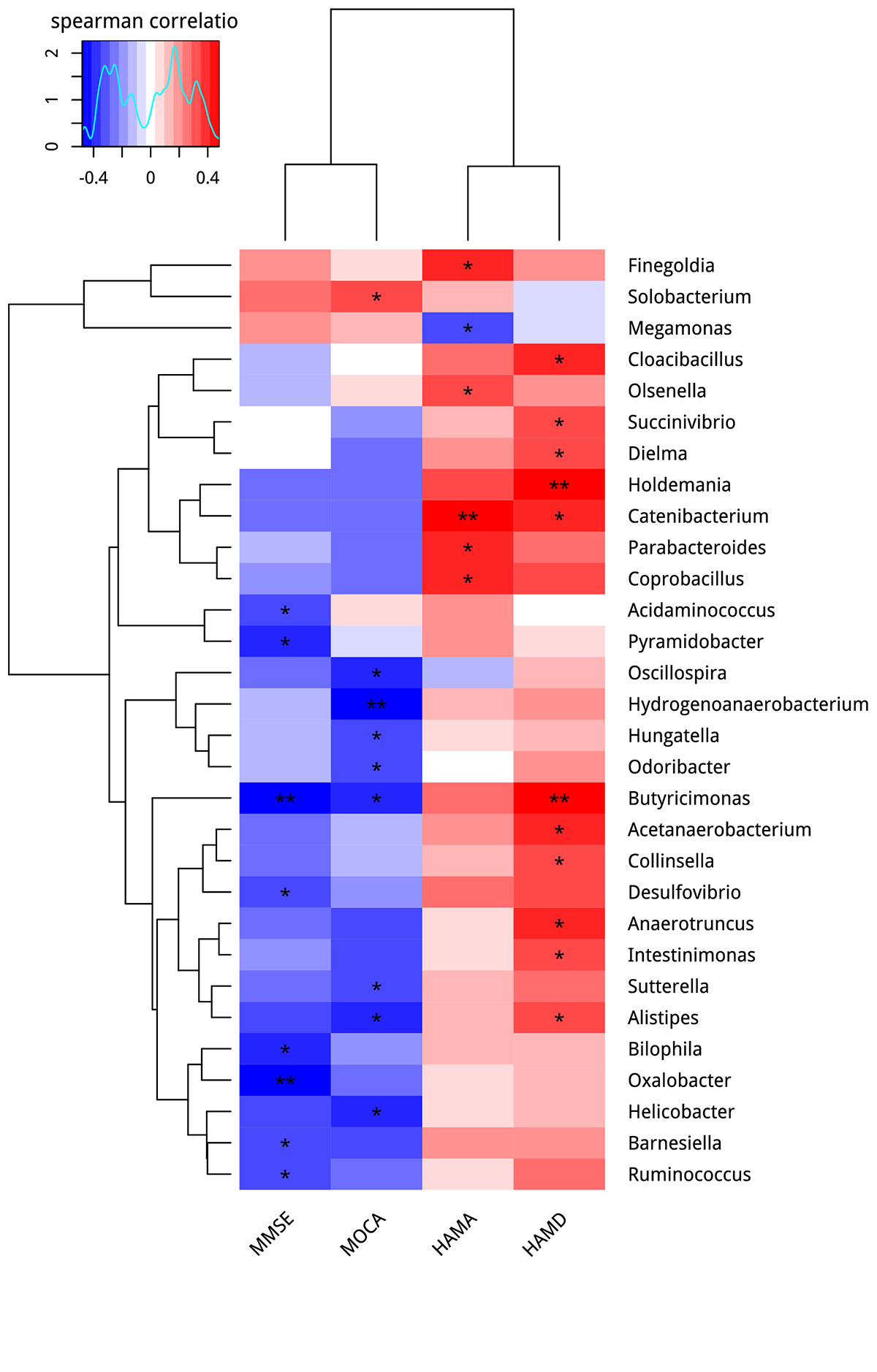
Results: There were significant differences between PD-MCI, PD-NC and healthy controls.After Linear Discriminant Analysis(LDA), 7 biomarker-microorganisms of PD-MCI were revealed: Rikenellaceae family-Alistipes genus, Barnesiella genus, Butyricimonas genus, Ruminococcus species, Klebsiella pneumoniae species, Ruminococcus torques species, Odoribacter splanchnicus species, which were more abundant in PD-MCI. Concentration of SCFA did not differ between cases and controls(Figure 1). Correlation analysis indicated that: 1) MMSE score positively correlated with the Barnesiella genus, Butyricimonas genus and Ruminococcus species ( p value = 0.0439; p value = 0.0022; p value = 0.0399) as well as isobutyric acid and isovaleric acid ( p value = 0.0203; p value = 0.0319) ; 2) MoCA score positively correlated with the Butyricimonas, Odoribacter and Alistipes genus ( p value = 0.0140; p value = 0.0397; p value = 0.0186)(Figure 2).
Conclusion: The result suggests that the qualitative or quantitative of intestinal microbiome were changed significantly in PD-MCI compared with PD-NC and HC. In keeping with recently published studies[1], Butyricimonas genus were more abundant in cases( p value = 0.0042). And the more abundance of Klebsiella pneumoniae species in PD-MCI was also an attractive finding( p value = 0.0145). Larger and further studies are warranted to elucidate the temporal and causal relationships between gut microbiota and PD with cognition decline and the suitability of the microbiome as a biomarker.
References: [1]Qian Y,Yang X,Xu S,Wu C,Song Y,Qin N,Chen SD,Xiao Q.Alteration of the fecal microbiota in Chinese patients with Parkinson’s disease.Brain Behav Immun.2018 70(2):194-202.
To cite this abstract in AMA style:
TZ. Ren, K. Nie, LJ. Wang. Gut microbiota in Parkinson disease with mild cognition impairment in a southern Chinese cohort. [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/gut-microbiota-in-parkinson-disease-with-mild-cognition-impairment-in-a-southern-chinese-cohort/. Accessed July 12, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/gut-microbiota-in-parkinson-disease-with-mild-cognition-impairment-in-a-southern-chinese-cohort/