Category: Allied Healthcare Professionals
Objective: Many neurological disorders often lead to various abnormal movements. Traditional assessment methods fail to accurately and objectively evaluate the affected muscles and the functional impairment. In this paper we reviewed the latest advances in the intelligent technologies which help clinicians qualitatively and quantitatively assess abnormal movement patterns and carry out personalized rehabilitation treatment.
Background: Individuals with neurological disorders often exhibit aberrant movements, i.e. deviation from the target trajectory caused by abnormal muscle synergies. These movements show mass and whole-extremity movements with limited joint separation [1]. Abnormal movements are classified into tremor, myoclonus, abnormal gait, parkinsonism and tics, based on phenomenology[2-4].
Method: A literature review was performed using the key words: “(movement or motion) and (assessment) and (technology or technique)” on Web of Science, Pubmed and Google Scholar on Sept 2 2023. The search criteria were studies that presented in decade 2013 to 2023.After reading the abstracts of the selected literatures, 9 abnormal motion pattern assessment instruments were selected and literature search was conducted again. The key word is “(Optical Motion Capture) and (abnormal movement)”and the search strategy was the same for the remaining eight instruments. The inclusion criteria were: studies that presented a intelligent assessment method for the assessment of abnormal movements caused by neurological diseases and was studied in patients or studies that presented newly developed techniques for assessing movement patterns but have not yet been used in clinical trials.
Results: Current intelligent assessment methods draw on optical motion capture, marker-less vision-based motion capture, radar technology, wearable inertial sensors, multi-lead electromyography, robotic feedback technology, ultrasound technology, infrared thermography and positron emission tomography (PET) / Single-Photon Emission Computed Tomography (SPECT) muscle metabolism imaging to accurately assess abnormal movements.
Conclusion: In this review, we provide an update of the latest equipment devices, summarizes what fine abnormal movement patterns can be assessed, what existing intelligent assessment methods can be used to distinguish abnormal movement patterns of different severity, and provide clear treatment directions for rehabilitation personnel.
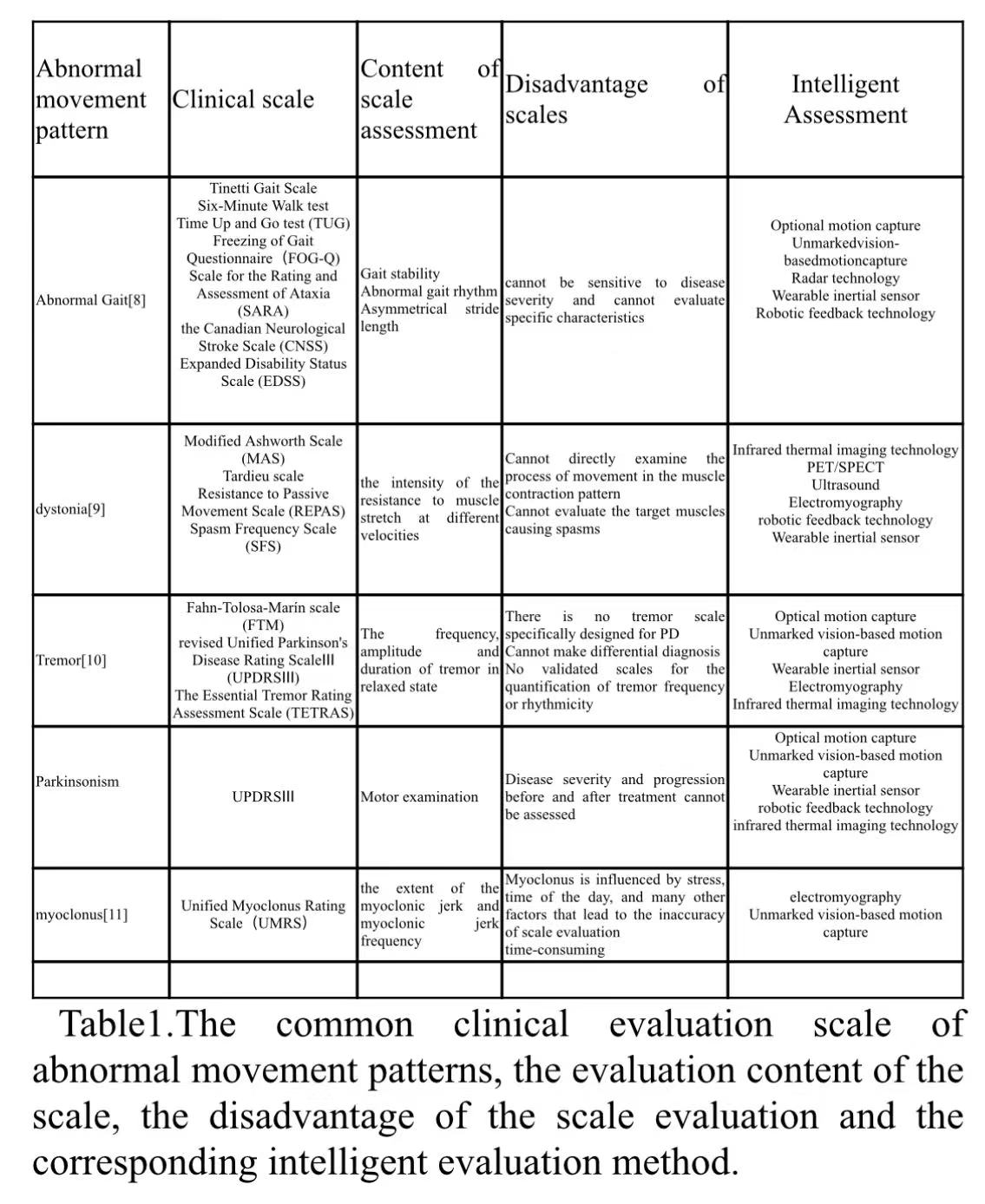
table1
References: Sethi A, Ting J, Allen M, Clark W, Weber D. Advances in motion and electromyography based wearable technology for upper extremity function rehabilitation: A review. J Hand Ther. 2020; 33(2): 180-7.
2. Mascia M M, Orofino G, Cimino P, Cadeddu G, Ercoli T, Defazio G. Writing tremor in Parkinson’s disease: frequency and associated clinical features. J Neural Transm (Vienna). 2022; 129(12): 1481-5.
3. Platz T. Evidence-Based Guidelines and Clinical Pathways in Stroke Rehabilitation-An International Perspective. Frontiers in Neurology. 2019; 10.
4. Hssayeni M D, Jimenez-Shahed J, Burack M A, Ghoraani B. Wearable Sensors for Estimation of Parkinsonian Tremor Severity during Free Body Movements. Sensors (Basel). 2019; 19(19).
5. Thenganatt M A,Louis E D. Distinguishing essential tremor from Parkinson’s disease: bedside tests and laboratory evaluations. Expert Rev Neurother. 2012; 12(6): 687-96.
6. Patrick E,Ada L. The Tardieu Scale differentiates contracture from spasticity whereas the Ashworth Scale is confounded by it. Clin Rehabil. 2006; 20(2): 173-82.
7. Ansari N N, Naghdi S, Hasson S, Azarsa M H, Azarnia S. The Modified Tardieu Scale for the measurement of elbow flexor spasticity in adult patients with hemiplegia. Brain Inj. 2008; 22(13-14): 1007-12.
8. Celik Y, Stuart S, Woo W L, Godfrey A. Gait analysis in neurological populations: Progression in the use of wearables. Med Eng Phys. 2021; 87: 9-29.
9. Howard I M,Patel A T. Spasticity evaluation and management tools. Muscle Nerve. 2023; 67(4): 272-83.
10. Elble R J,Ondo W. Tremor rating scales and laboratory tools for assessing tremor. J Neurol Sci. 2022; 435: 120202.
11. Hyppönen J, Hakala A, Annala K, Zhang H, Peltola J, Mervaala E, Kälviäinen R. Automatic assessment of the myoclonus severity from videos recorded according to standardized Unified Myoclonus Rating Scale protocol and using human pose and body movement analysis. Seizure. 2020; 76: 72-8.
12. Herda L, Fua P, Plänkers R, Boulic R, Thalmann D. Using skeleton-based tracking to increase the reliability of optical motion capture. Hum Mov Sci. 2001; 20(3): 313-41.
13. McHugh B, Akhbari B, Morton A M, Moore D C, Crisco J J. Optical motion capture accuracy is task-dependent in assessing wrist motion. J Biomech. 2021; 120: 110362.
14. Smirnova V, Khamatnurova R, Kharin N, Yaikova E, Baltina T, Sachenkov O. The Automatization of the Gait Analysis by the Vicon Video System: A Pilot Study. Sensors (Basel). 2022; 22(19).
15. Lee K D,Park H S. Real-Time Motion Analysis System Using Low-Cost Web Cameras and Wearable Skin Markers. Front Bioeng Biotechnol. 2021; 9: 790764.
16. Wang L, Li Y, Xiong F, Zhang W. Gait Recognition Using Optical Motion Capture: A Decision Fusion Based Method. Sensors (Basel). 2021; 21(10).
17. Fonk R, Schneeweiss S, Simon U, Engelhardt L. Hand Motion Capture from a 3D Leap Motion Controller for a Musculoskeletal Dynamic Simulation. Sensors (Basel). 2021; 21(4).
18. Klöpfer-Krämer I, Brand A, Wackerle H, Müßig J, Kröger I, Augat P. Gait analysis – Available platforms for outcome assessment. Injury. 2020; 51 Suppl 2: S90-s6.
19. Litinas K, Roenigk K L, Daly J J. Thigh and Shank, Kinetic and Potential Energies during Gait Swing Phase in Healthy Adults and Stroke Survivors. Brain Sci. 2022; 12(8).
20. Xie Q, Sheng B, Huang J, Zhang Q, Zhang Y. A Pilot Study of Compensatory Strategies for Reach-to-Grasp-Pen in Patients with Stroke. Appl Bionics Biomech. 2022; 2022: 6933043.
21. Johansson G M, Grip H, Levin M F, Häger C K. The added value of kinematic evaluation of the timed finger-to-nose test in persons post-stroke. J Neuroeng Rehabil. 2017; 14(1): 11.
22. Khwaounjoo P, Singh G, Grenfell S, Özsoy B, MacAskill M R, Anderson T J, Çakmak Y O. Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor. Sensors (Basel). 2022; 22(12).
23. Colyer S L, Evans M, Cosker D P, Salo A I T. A Review of the Evolution of Vision-Based Motion Analysis and the Integration of Advanced Computer Vision Methods Towards Developing a Markerless System. Sports Med Open. 2018; 4(1): 24.
24. Ripic Z, Nienhuis M, Signorile J F, Best T M, Jacobs K A, Eltoukhy M. A comparison of three-dimensional kinematics between markerless and marker-based motion capture in overground gait. J Biomech. 2023; 159: 111793.
25. Dilek E,Dener M. Computer Vision Applications in Intelligent Transportation Systems: A Survey. Sensors (Basel). 2023; 23(6).
26. van der Velden B H M, Kuijf H J, Gilhuijs K G A, Viergever M A. Explainable artificial intelligence (XAI) in deep learning-based medical image analysis. Med Image Anal. 2022; 79: 102470.
27. Kanko R M, Laende E K, Davis E M, Selbie W S, Deluzio K J. Concurrent assessment of gait kinematics using marker-based and markerless motion capture. J Biomech. 2021; 127: 110665.
28. Zhao Y, Li J, Wang X, Liu F, Shan P, Li L, Fu Q. A Lightweight Pose Sensing Scheme for Contactless Abnormal Gait Behavior Measurement. Sensors (Basel). 2022; 22(11).
29. Young F, Mason R, Morris R, Stuart S, Godfrey A. Internet-of-Things-Enabled Markerless Running Gait Assessment from a Single Smartphone Camera. Sensors (Basel). 2023; 23(2).
30. Kim B,Neville C. Accuracy and feasibility of a novel fine hand motor skill assessment using computer vision object tracking. Sci Rep. 2023; 13(1): 1813.
31. Faity G, Mottet D, Froger J. Validity and Reliability of Kinect v2 for Quantifying Upper Body Kinematics during Seated Reaching. Sensors (Basel). 2022; 22(7).
32. Knippenberg E, Verbrugghe J, Lamers I, Palmaers S, Timmermans A, Spooren A. Markerless motion capture systems as training device in neurological rehabilitation: a systematic review of their use, application, target population and efficacy. J Neuroeng Rehabil. 2017; 14(1): 61.
33. Eltoukhy M, Oh J, Kuenze C, Signorile J. Improved kinect-based spatiotemporal and kinematic treadmill gait assessment. Gait Posture. 2017; 51: 77-83.
34. Bakhti K K A, Laffont I, Muthalib M, Froger J, Mottet D. Kinect-based assessment of proximal arm non-use after a stroke. J Neuroeng Rehabil. 2018; 15(1): 104.
35. Zhang Z, Hong R, Lin A, Su X, Jin Y, Gao Y, Peng K, Li Y, Zhang T, Zhi H, Guan Q, Jin L. Automated and accurate assessment for postural abnormalities in patients with Parkinson’s disease based on Kinect and machine learning. J Neuroeng Rehabil. 2021; 18(1): 169.
36. Hong R, Zhang T, Zhang Z, Wu Z, Lin A, Su X, Jin Y, Gao Y, Peng K, Li L, Pan L, Zhi H, Guan Q, Jin L. A summary index derived from Kinect to evaluate postural abnormalities severity in Parkinson’s Disease patients. NPJ Parkinsons Dis. 2022; 8(1): 96.
37. Wu Z, Hong R, Li S, Peng K, Lin A, Gao Y, Jin Y, Su X, Zhi H, Guan Q, Pan L, Jin L. Technology-based therapy-response evaluation of axial motor symptoms under daily drug regimen of patients with Parkinson’s disease. Front Aging Neurosci. 2022; 14: 901090.
38. Rupprechter S, Morinan G, Peng Y, Foltynie T, Sibley K, Weil R S, Leyland L A, Baig F, Morgante F, Gilron R, Wilt R, Starr P, Hauser R A, O’Keeffe J. A Clinically Interpretable Computer-Vision Based Method for Quantifying Gait in Parkinson’s Disease. Sensors (Basel). 2021; 21(16).
39. Steffensen E A, Magalhães F, Knarr B A, Kingston D C. Comparison of markerless and marker-based motion capture of gait kinematics in individuals with cerebral palsy and chronic stroke: A case study series. Res Sq. 2023.
40. Du H, Henry P, Ren X, Cheng M, Goldman D B, Seitz S M, Fox D. Interactive 3D modeling of indoor environments with a consumer depth camera. in Proceedings of the 13th international conference on Ubiquitous computing. 2011; Association for Computing Machinery: Beijing, China. p. 75–84.
41. Zhu Y, Lu W, Gan W, Hou W. A contactless method to measure real-time finger motion using depth-based pose estimation. Comput Biol Med. 2021; 131: 104282.
42. Kincaid C J, Vaterlaus A C, Stanford N R, Charles S K. Frequency response of the leap motion controller and its suitability for measuring tremor. Med Eng Phys. 2019; 63: 72-8.
43. Liu W, Lin X, Chen X, Wang Q, Wang X, Yang B, Cai N, Chen R, Chen G, Lin Y. Vision-based estimation of MDS-UPDRS scores for quantifying Parkinson’s disease tremor severity. Med Image Anal. 2023; 85: 102754.
44. Guo Z, Zeng W, Yu T, Xu Y, Xiao Y, Cao X, Cao Z. Vision-Based Finger Tapping Test in Patients With Parkinson’s Disease via Spatial-Temporal 3D Hand Pose Estimation. IEEE J Biomed Health Inform. 2022; 26(8): 3848-59.
45. Zhang Z, Pouliquen P O, Waxman A, Andreou A G. Acoustic micro-Doppler radar for human gait imaging. J Acoust Soc Am. 2007; 121(3): El110-3.
46. Seifert A K, Grimmer M, Zoubir A M. Doppler Radar for the Extraction of Biomechanical Parameters in Gait Analysis. IEEE J Biomed Health Inform. 2021; 25(2): 547-58.
47. Seifert A K, Amin M G, Zoubir A M. Toward Unobtrusive In-Home Gait Analysis Based on Radar Micro-Doppler Signatures. IEEE Trans Biomed Eng. 2019; 66(9): 2629-40.
48. Jiang X, Zhang Y, Yang Q, Deng B, Wang H. Millimeter-Wave Array Radar-Based Human Gait Recognition Using Multi-Channel Three-Dimensional Convolutional Neural Network. Sensors (Basel). 2020; 20(19).
49. Soubra R, Mourad-Chehade F, Chkeir A. Automation of the Timed Up and Go Test Using a Doppler Radar System for Gait and Balance Analysis in Elderly People. J Healthc Eng. 2023; 2023: 2016262.
50. Liang X, Deng J, Zhang H, Gulliver T A. Ultra-Wideband Impulse Radar Through-Wall Detection of Vital Signs. Scientific Reports. 2018; 8(1): 13367.
51. Yim D, Lee W H, Kim J I, Kim K, Ahn D H, Lim Y H, Cho S H, Park H K, Cho S H. Quantified Activity Measurement for Medical Use in Movement Disorders through IR-UWB Radar Sensor. Sensors (Basel). 2019; 19(3).
52. Na J Y, Lee W H, Lim Y H, Cho S H, Cho S H, Park H K. Early screening tool for developmental delay in infancy: Quantified assessment of movement asymmetry using IR-UWB radar. Front Pediatr. 2022; 10: 731534.
53. Zilani T A, Al-Turjman F, Khan M B, Zhao N, Yang X. Monitoring Movements of Ataxia Patient by Using UWB Technology. Sensors (Basel). 2020; 20(3).
54. Faisal A I, Majumder S, Mondal T, Cowan D, Naseh S, Deen M J. Monitoring Methods of Human Body Joints: State-of-the-Art and Research Challenges. Sensors (Basel). 2019; 19(11).
55. Wang Q, Markopoulos P, Yu B, Chen W, Timmermans A. Interactive wearable systems for upper body rehabilitation: a systematic review. Journal of NeuroEngineering and Rehabilitation. 2017; 14(1): 20.
56. Ricci L, Taffoni F, Formica D. On the Orientation Error of IMU: Investigating Static and Dynamic Accuracy Targeting Human Motion. PLoS One. 2016; 11(9): e0161940.
57. Friesen K B, Sigurdson A, Lang A E. Comparison of scapular kinematics from optical motion capture and inertial measurement units during a work-related and functional task protocol. Med Biol Eng Comput. 2023.
58. Teufl W, Miezal M, Taetz B, Fröhlich M, Bleser G. P 052 – Detection of lower extremity asymmetries in slow and dynamic bilateral tasks. Inertial Sensor system vs Optical Motion Capture System. Gait Posture. 2022; 95: 219-20.
59. Slade P, Habib A, Hicks J L, Delp S L. An Open-Source and Wearable System for Measuring 3D Human Motion in Real-Time. IEEE Trans Biomed Eng. 2022; 69(2): 678-88.
60. Duan L T, Lawo M, Wang Z G, Wang H Y. Human Lower Limb Motion Capture and Recognition Based on Smartphones. Sensors (Basel). 2022; 22(14).
61. Yang Y, Chen L, Pang J, Huang X, Meng L, Ming D. Validation of a Spatiotemporal Gait Model Using Inertial Measurement Units for Early-Stage Parkinson’s Disease Detection During Turns. IEEE Trans Biomed Eng. 2022; 69(12): 3591-600.
62. Zumaeta K, Romero S E, Torres E, Urdiales L, Ramirez A, Camargo I, Lizarraga K J, Castaneda B. Combining inertial sensors and optical flow to assess finger movements: Pilot study for telehealth applications. Annu Int Conf IEEE Eng Med Biol Soc. 2021; 2021: 2409-12.
63. Lee J, Park S, Shin H. Detection of Hemiplegic Walking Using a Wearable Inertia Sensing Device. Sensors (Basel). 2018; 18(6).
64. Kim H B, Lee H J, Lee W W, Kim S K, Jeon H S, Park H Y, Shin C W, Yi W J, Jeon B, Park K S. Validation of Freezing-of-Gait Monitoring Using Smartphone. Telemed J E Health. 2018; 24(11): 899-907.
65. Abdollahi M, Kuber P M, Hoang C, Shiraishi M, Soangra R, Rashedi E. Kinematic Assessment of Turning and Walking Tasks Among Stroke Survivors by Employing Wearable Sensors and Pressure Platform. Annu Int Conf IEEE Eng Med Biol Soc. 2021; 2021: 6635-8.
66. Lin B S, Lee I J, Hsiao P C, Yang S Y, Chen C Y, Lee S H, Huang Y F, Yen M H, Hu Y H. Design of a Multi-Sensor System for Exploring the Relation between Finger Spasticity and Voluntary Movement in Patients with Stroke. Sensors (Basel). 2022; 22(19).
67. Amit M, Yalcin C, Liu J, Skalsky A J, Garudadri H, Ng T N. Multimodal assessment of spasticity using a point-of-care instrumented glove to separate neural and biomechanical contributions. iScience. 2022; 25(11): 105286.
68. Jeon H, Lee W, Park H, Lee H J, Kim S K, Kim H B, Jeon B, Park K S. Automatic Classification of Tremor Severity in Parkinson’s Disease Using a Wearable Device. Sensors (Basel). 2017; 17(9).
69. Fuchs C, Nobile M S, Zamora G, Degeneffe A, Kubben P, Kaymak U. Tremor assessment using smartphone sensor data and fuzzy reasoning. BMC Bioinformatics. 2021; 22(Suppl 2): 57.
70. Sigcha L, Pavón I, Costa N, Costa S, Gago M, Arezes P, López J M, Arcas G. Automatic Resting Tremor Assessment in Parkinson’s Disease Using Smartwatches and Multitask Convolutional Neural Networks. Sensors (Basel). 2021; 21(1).
To cite this abstract in AMA style:
YJ. Bao, RH. Hong, WT. Qin, Z. Wu, YP. Song, LJ. Jin. Intelligent Assessment of Abnormal Movements in Neurological Disorders: An Update [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/intelligent-assessment-of-abnormal-movements-in-neurological-disorders-an-update/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/intelligent-assessment-of-abnormal-movements-in-neurological-disorders-an-update/