Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To evaluate the range and motor state during sleep of PD patients by using subjective scale-based assessment as well as PKG. To evaluate the range and motor state during sleep of PD patients by using subjective scale-based assessment as well as PKG.
Background: Nighttime symptoms are equally important to quality of life in Parkinson’s disease (PD) but rarely incorporated within the management plans in real life clinics. Clinical reporting of nighttime symptoms remains suboptimal, and the use of PD validated wearable sensors, such as the Parkinson’s kinetigraph (PKG), may offer a useful surrogate.
Method: Data from the Kings College London, PKG registry were used and 112 PD patients were enrolled in this observational, retrospective audit. A group of 11 PD patients undergoing advanced therapy were also analysed. The clinical assessment of sleep was done with PD Sleep Scale (PDSS) and Epworth Sleepiness Scale (ESS), with cutoff of PDSS score < 100 as indicative of disturbed sleep. PD treatment prescribed after 8 pm was considered nighttime medication. PKGs with minimum 4 nights recorded were taken into consideration. Based on Nocturnal Bradykinesia (NBK) scores provided by the PKG manufacturer and a local algorithm, patients were divided into 3 groups: mild, moderate, and severe NBK.
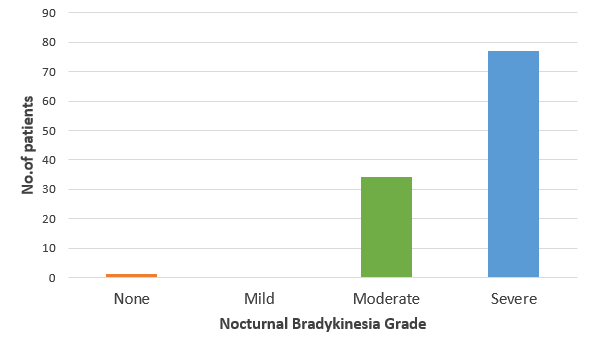
Results: None had mild NBK, 30.35% fell in the moderate, 68.75% in the severe NBK range and only 1 patient showed normal range of motion. 34.82% scored below 100 on the PDSS. More than half of these patients (61.53%) had severe NBK picked up by the PKG. The same cohort had higher ESS scores (11.28 ± 6.21 vs 5.74 ± 4.52, p < 0.01) and higher LEDD (736.3mg ± 321.48mg vs 562.67mg ± 336.64mg, p < 0,01), compared to the PDSS ≥100 group. 64.3% had nighttime PD medication prescribed. No correlation was found between NBK grade and LEDD, Hoehn & Yahr stage and disease duration, while a very weak negative correlation was noted between NBK grade and nighttime medication (r = -0.04). From the advanced therapy group, 8 (72.72%) showed severe NBK on the PKG recording.
Conclusion: Sleep disorders remain common in PD and are associated with significant nighttime bradykinesia. In over 35% there is clinical correlation as indicated by PDSS scores as well as the LEDD. We suggest the clinical application of wearable sensors for effective nighttime monitoring and to move away from the “clinical only” tunnel vision approach.
The distribution of NBK grades
To cite this abstract in AMA style:
I. Murasan, M. Qamar, K. Poplawska-Domaszewicz, D. Trivedi, K R. Chaudhuri, C. Falup-Pecurariu. Nocturnal Bradykinesia is better detected using wearable sensors in Parkinson’s disease compared to clinical outcome [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/nocturnal-bradykinesia-is-better-detected-using-wearable-sensors-in-parkinsons-disease-compared-to-clinical-outcome/. Accessed July 3, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/nocturnal-bradykinesia-is-better-detected-using-wearable-sensors-in-parkinsons-disease-compared-to-clinical-outcome/