Category: Parkinsonism, Others
Objective: Defining the burden of non-motor symptoms in Primary Familial Brain Calcification
Background: PFBC is a rare neurodegenerative disorder of adulthood characterized by calcium deposition in basal ganglia and other brain areas; in 50% of subjects a genetic mutation can be found (SLC20A2, PDGFB, PDGFRB, XPR1, MYORG, JAM2, CMPK2, NAA60). The main clinical manifestations include movement disorders (mainly parkinsonism), cognitive or psychiatric disturbances. Except for headache and psychiatric manifestations, other non-motor symptoms have not been dissected in PFBC. COMPASS-31 is dysautonomia scale that has already been validated in other forms of parkinsonism
Method: CT scans, clinical and genetic (NGS) and neuropsychological evaluation, COMPASS-31 administration; secondary causes of brain calcifications were excluded through blood tests
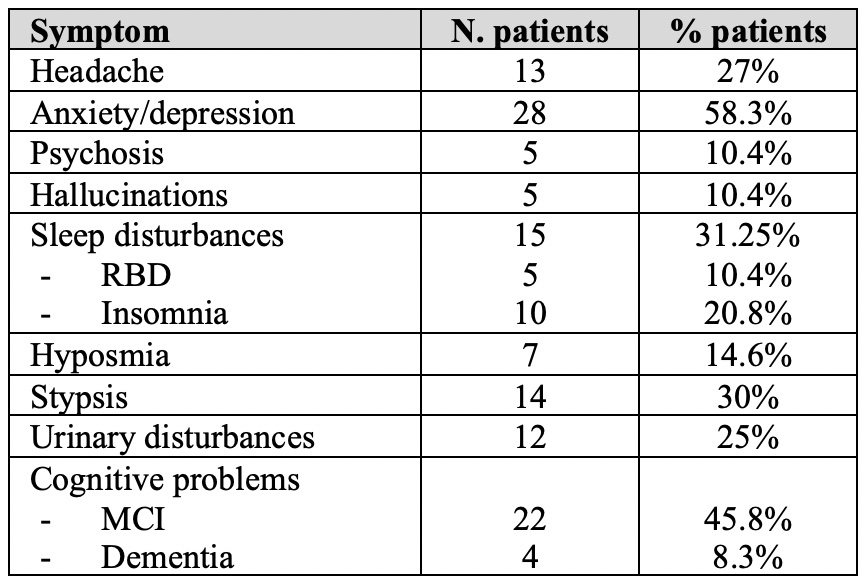
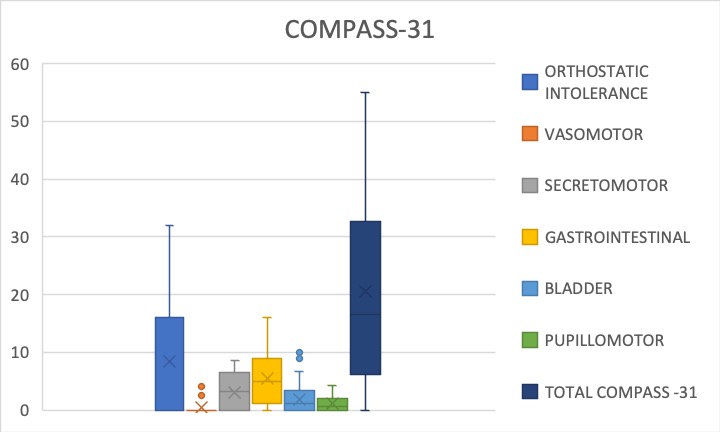
Results: 48 PFBC patients were recruited; genetic test resulted negative in 23, 10 had SLC20A2 mutations, 6 MYORG, 3 PDGFB, 1 PDGFRB, 2 heterozygous JAM2, 3 are ongoing. Mean total calcification score at CT scan was 21.2. The most frequent motor manifestation was parkinsonism in 56%. Non motor symptoms were assessed (Table I): anxiety or depression were the most frequent complaint (58%) and 5 subjects reported psychosis, hallucinations or OCD. Headache was found in 27% and sleep disturbances in 31%; typical PD related non-motor symptoms such as hyposmia and constipation were also frequent even in patients without motor involvement; urinary disturbances or incontinence were reported in 25% of subjects. Neuropsychological assessment revealed cognitive (MCI or dementia in 26 patients (visuospatial domain, attention, language and executive functions were most involved). COMPASS-31 mean score was 20.5 (Fig.1), with higher sub-scores in items related to orthostatic intolerance (8.3) and gastrointestinal problems (5.5). No clear differences could be detected based on genetic subgroups or among patients with or without motor symptoms, but MYORG patients tended to higher total score compared to SLC20A2, as well as patients with cognitive decline compared to those with normal cognitive function
Conclusion: The presence of non-motor symptoms is frequent in PFBC and should be systematically assessed to better meet patients’ needs
Table I
Fig.1
References: Balck A, Schaake S, Kuhnke NS, et al. Genotype-Phenotype Relations in Primary Familial Brain Calcification: Systematic MDSGene Review. Mov Disord. 2021;36(11):2468-2480. doi:10.1002/mds.28753
To cite this abstract in AMA style:
G. Bonato, M. Carecchio. Non motor symptoms assessment in Primary Familial Brain Calcification, survey on a cohort [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/non-motor-symptoms-assessment-in-primary-familial-brain-calcification-survey-on-a-cohort/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/non-motor-symptoms-assessment-in-primary-familial-brain-calcification-survey-on-a-cohort/