Session Information
Date: Saturday, October 6, 2018
Session Title: Cognitive Disorders
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: In this study, we have tried to find any correlation between severity of cognitive dysfunction and parkinsonism in NPH patients & to look for any novel phenotypic subclassification if any.
Background: Normal pressure hydrocephalus (NPH) is not only an important treatable cause of dementia in the elderly population but also an important entity in the list of differential diagnosis of degenerative atypical parkinsonism.
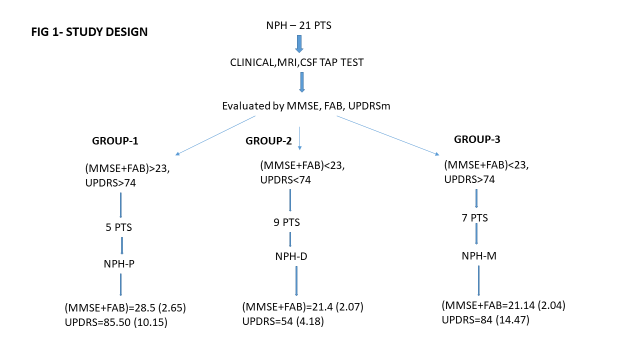
Methods: In this cross-sectional hospital-based study, we have evaluated 21 NPH patients with clinical, radiological & CSF tap test, followed by MMSE, FAB & UPDRS-MOTOR scale scoring. After this, we have tried to subclassify the patients depending on (MMSE+FAB) and UPDRS-MOTOR score.
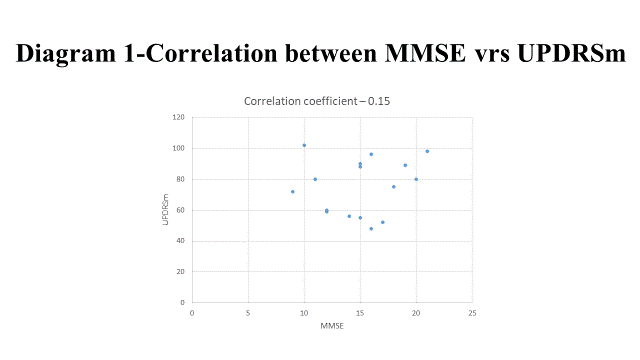
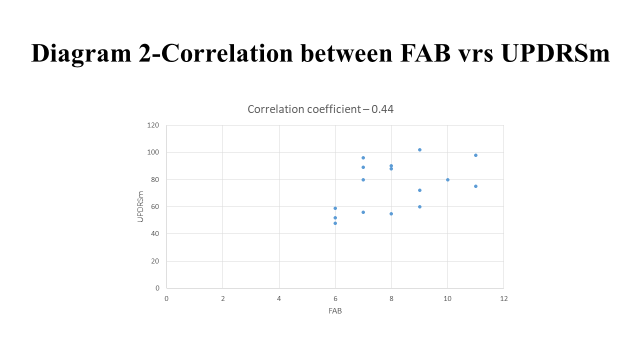
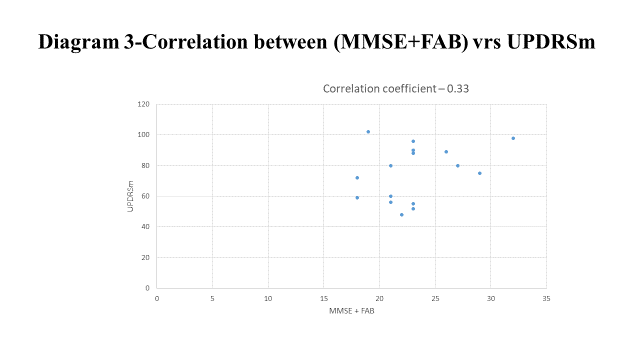
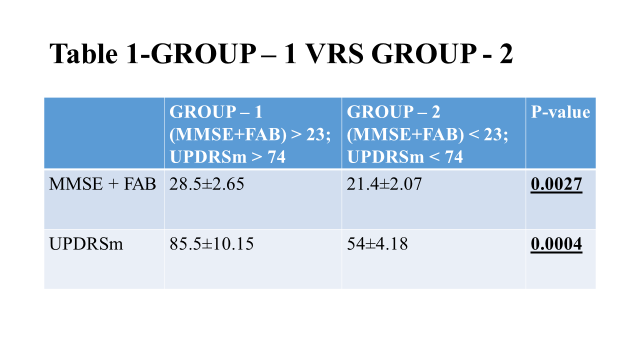
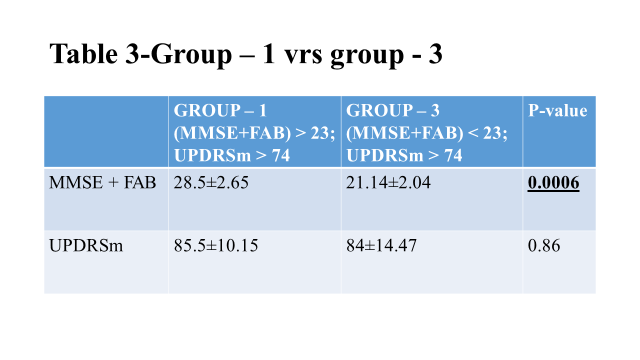
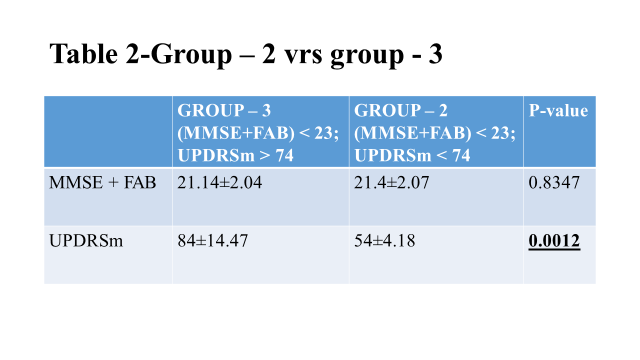
Results: The mean±SD of MMSE, FAB, (MMSE+FAB) & UPDRS-MOTOR score in 21 NPH pts (13 males, 8 female) are 15±3.54, 8.06±1.65, 23.06±3.84 & 74.25±19.04 respectively (fig-1). Correlation coefficient between MMSE, FAB, (MMSE+FAB) and UPDRS-MOTOR score are 0.15 (diag-1), 0.44 (diag-2) & 0.33 (diag-3) respectively. Taking cut-off as 23 & 74 (as these are the population mean) for (MMSE+FAB) & UPDRS-MOTOR score respectively we divided the population into three groups: NPH-P (group-1), NPH-D (group-2) & NPH-M (group-3). Statistically, a significant difference exists between NPH-D (54±4.18) & NPH-M (84±14.47) (table-2) (P-0.0012) when UPDRS-MOTOR score was considered, but none between NPH-M & NPH-P (85.5±10.15) group (table-3) (P-0.86). The (MMSE+FAB) score shows significant difference between NPH-P (28.5±2.65) & NPH-M (21.14±2.04) group (table-3) (P -0.0006), but not between NPH-D(21.4±2.07) & NPH-M group (table-2) (P-0.83).
Conclusions: There is no significant correlation between cognitive dysfunction severity and parkinsonian severity in NPH patients, but FAB score (correlation coefficient-0.44) correlate more with UPDRS-MOTOR score than the MMSE score (correlation coefficient-0.15). But depending on the severity, they can be subclassified as NPH-P with severe parkinsonism, NPH-D with predominant dementia, and NPH-M with both severe parkinsonism and dementia.
References: 1. Molde K, Söderström L, Laurell K. Parkinsonian symptoms in normal pressure hydrocephalus: a population-based study. J Neurol. 2017; 264(10): 2141–2148. doi: 10.1007/s00415-017-8598-5. 2. Kang K, Jeon JS, Kim T, Choi D, Ko PW, Hwang SK, Lee HW. Asymmetric and Upper Body Parkinsonism in Patients with Idiopathic Normal-Pressure Hydrocephalus. J Clin Neurol. 2016 Oct;12(4):452-459. doi: 10.3988/jcn.2016.12.4.452.
To cite this abstract in AMA style:
A. Acharya, A. Biswas, S. Das. Parkinsonism & Cognitive Dysfunction Severity Correlation in NPH with a Suggested Novel Phenotypic Subclassifcation of NPH [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/parkinsonism-cognitive-dysfunction-severity-correlation-in-nph-with-a-suggested-novel-phenotypic-subclassifcation-of-nph/. Accessed July 9, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/parkinsonism-cognitive-dysfunction-severity-correlation-in-nph-with-a-suggested-novel-phenotypic-subclassifcation-of-nph/