Category: Epidemiology
Objective: To investigate the aetiology of PD demographically in an under researched region.
Background: PD monogenic and susceptibility risk factors explain little to none of the disease in Sub Saharan Africa (SSA) [1]. A polymorphism in the GBA1 gene was recently identified in whole genome screen in West-African and African-American patients [2,3]. Conversely populations with little to no PD may say something about absence of exposure to risk factors.
Method: One of the aims of The Transforming Parkinson’s Care in Africa (TraPCAf) multinational study is to study environmental and genetic risk factors [4]. In this framework 112 late onset PD outpatients at Kilimanjaro Christian Medical Centre in Moshi Tanzania were analysed. Inspired by a relative absence of pastoralist nomads among the hospital PD cohort, the Hadzabe tribe in a remote area nearby the Serengeti was investigated. They live off the land with bow and arrow, their diet consisting of any edible animal, berries and tubers. Healthcare workers and researchers working with the tribe in the wider region were asked about any Hadzabe with PD symptoms.
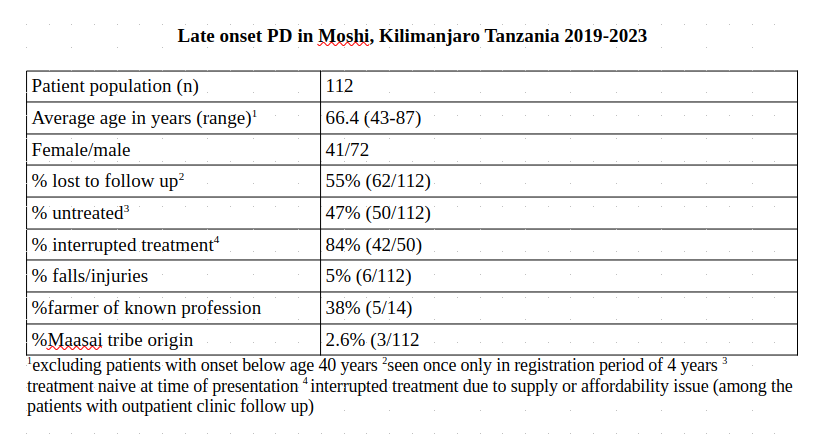
Results: Characteristics were largely comparable to SSA populations elsewhere [table1]. A higher than average rate of healthcare insured individuals was explained by the hospital setting. Loss to follow up and off treatment state persisted among patients even with healthcare insurance. A conspicuously low rate of falls among PD complications is seen in this population where most patients are smallholder farmers who continue to walk to and work their land because it generates food and income. Only 3 patients were of Maasai origin, a significant under representation for a hospital being the referral hospital for Maasailand. No cases of PD have been seen by any of the local healthcare workers and researchers monitoring this hunter gatherer tribe up to 4-5 decades back [figure1].
Conclusion: The treatment gap likely represents a broader phenomenon of lagging utilisation of diagnostic and therapeutic opportunities in a socioculturally stigmatised disorder and can still improve over time [1,5]. The absence of PD in certain (semi)nomadic tribes calls for novel hypothesis construction regarding their outdoors nomadic lifestyle, ranging from genetic selection to lack of use of pesticides. Information regarding ethnic origin may remain relevant as long as the origins of PD elude us.
Late onset PD in Kilimanjaro
Tribes with no/very little Parkinson’s Disease
References: [1] Dekker MCJ, Coulibaly T, Bardien S, Ross OA, Carr J, Komolafe M. Parkinson’s Disease Research on the African Continent: Obstacles and Opportunities. Front Neurol. 2020 Jun 19;11:512. doi: 10.3389/fneur.2020.00512. PMID: 32636796; PMCID: PMC7317302.
[2] Rizig M, Bandres-Ciga S, Makarious MB, Ojo OO, Crea PW, Abiodun OV, Levine KS, Abubakar SA, Achoru CO, Vitale D, Adeniji OA, Agabi OP, Koretsky MJ, Agulanna U, Hall DA, Akinyemi RO, Xie T, Ali MW, Shamim EA, Ani-Osheku I, Padmanaban M, Arigbodi OM, Standaert DG, Bello AH, Dean MN, Erameh CO, Elsayed I, Farombi TH, Okunoye O, Fawale MB, Billingsley KJ, Imarhiagbe FA, Jerez PA, Iwuozo EU, Baker B, Komolafe MA, Malik L, Nwani PO, Daida K, Nwazor EO, Miano-Burkhardt A, Nyandaiti YW, Fang ZH, Obiabo YO, Kluss JH, Odeniyi OA, Hernandez DG, Odiase FE, Tayebi N, Ojini FI, Sidranksy E, Onwuegbuzie GA, D’Souza AM, Osaigbovo GO, Berhe B, Osemwegie N, Reed X, Oshinaike OO, Leonard HL, Otubogun FM, Alvarado CX, Oyakhire SI, Ozomma SI, Samuel SC, Taiwo FT, Wahab KW, Zubair YA, Iwaki H, Kim JJ, Morris HR, Hardy J, Nalls MA, Heilbron K, Norcliffe-Kaufmann L; Nigeria Parkinson Disease Research Network; International Parkinson’s Disease Genomics Consortium Africa; Black and African American Connections to Parkinson’s Disease Study Group; 23andMe Research Team; Blauwendraat C, Houlden H, Singleton A, Okubadejo NU (2023) Identification of genetic risk loci and causal insights associated with Parkinson’s disease in African and African admixed populations: a genome-wide association study. Lancet Neurology 22, 1015-1025. https://doi.org/10.1016/S1474-4422(23)00283-1.
[3] Towns C, Richer M, Jasaityte S, Stafford EJ, Joubert J, Antar T, Martinez-Carrasco A, Makarious MB, Casey B, Vitale D, Levine K, Leonard H, Pantazis CB, Screven LA, Hernandez DG, Wegel CE, Solle J, Nalls MA, Blauwendraat C, Singleton AB, Tan MMX, Iwaki H, Morris HR; Global Parkinson’s Genetics Program (GP2). Defining the causes of sporadic Parkinson’s disease in the global Parkinson’s genetics program (GP2). NPJ Parkinsons Dis. 2023 Sep 12;9(1):131. doi: 10.1038/s41531-023-00533-w. PMID: 37699923; PMCID: PMC10497609.
[4] Walker R, Fothergill-Misbah N, Kariuki S, Ojo O, Cilia R, Dekker MCJ, Agabi O, Akpalu A, Amod F, Breckons M, Cham M, Del Din S, Dotchin C, Guggsa S, Kwasa J, Mushi D, Nwaokorie FO, Park T, Rochester L, Rogathi J, Sarfo FS, Shalash A, Ternent L, Urasa S, Okubadejo N. Transforming Parkinson’s Care in Africa (TraPCAf): protocol for a multimethodology National Institute for Health and Care Research Global Health Research Group project. BMC Neurol. 2023 Oct 19;23(1):373. doi: 10.1186/s12883-023-03414-0. PMID: 37858118; PMCID: PMC10585779.
[5] Dotchin C, Msuya O, Kissima J, Massawe J, Mhina A, Moshy A, Aris E, Jusabani A, Whiting D, Masuki G, Walker R (2008)The prevalence of Parkinson’s disease in rural Tanzania. Mov Disord 23, 1567-672. doi: 10.1002/mds.21898. PMID: 18581482.
To cite this abstract in AMA style:
S. Urasa, W. Howlett, R. Walker, M. Dekker. PD in Tanzania: representative in city dwellers, absent in nomadic tribespeople? [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/pd-in-tanzania-representative-in-city-dwellers-absent-in-nomadic-tribespeople/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/pd-in-tanzania-representative-in-city-dwellers-absent-in-nomadic-tribespeople/