Session Information
Date: Saturday, October 6, 2018
Session Title: Surgical Therapy: Parkinson's Disease
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: Increasing worldwide utilization of Deep Brain Stimulation (DBS) for movement disorders and other diseases has increased demand for this therapy from a larger population of patients. Evaluation of these patients for candidacy and post treatment demands has been challenging to predict. This study is aimed at improving ability to predict risk based on discrete pre-operative factors to help patients, providers and health care systems in directing care around DBS therapy.
Background: Surgeons are not able to accurately predict the clinical status of a patient after DBS surgery. Furthermore, clinical decision making is susceptible to biases. Clinical decision making can be improved with the application of predictive models and decision support systems (DSS). The purpose of this study was to develop a risk stratification model and DSS that could accurately predict whether a patient was likely to be of high- or low-acuity discharge disposition (DD) status after DBS surgery, based on routinely measured preoperative variables.
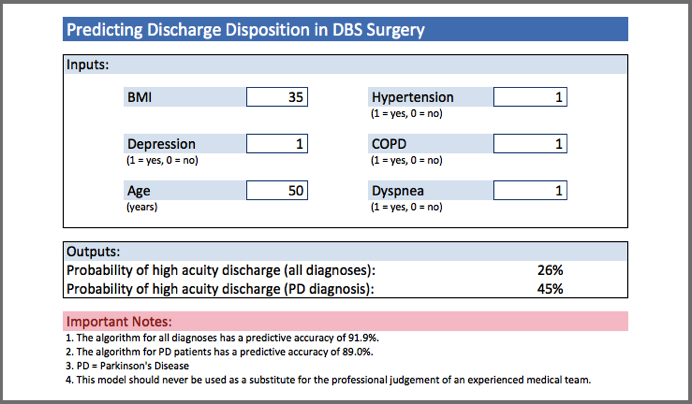
Methods: Data were collected for 135 DBS patients by reviewing medical records. Logistic regression analysis was applied to develop the predictive algorithm based on patient demographic parameters and co-morbidities. A DSS was developed that could estimate the likelihood of a patient experiencing high-acuity DD status postoperatively.
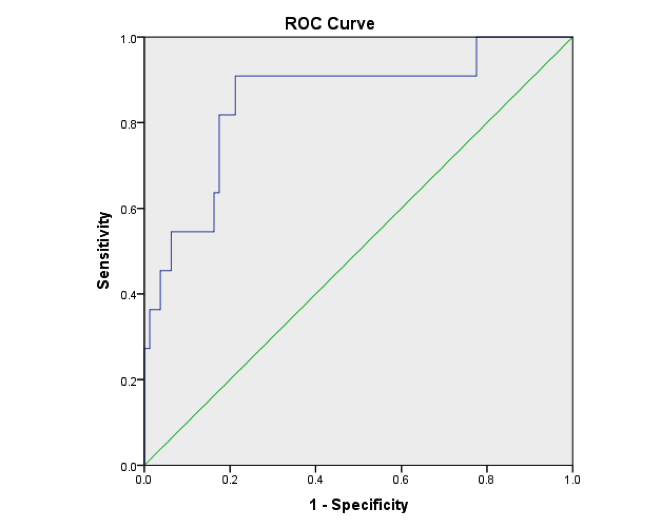
Results: Two predictive models were significant. They showed good fit, and were calibrated by using AUROC curve analysis. The model predicting DD in all patients (n=135) yielded a predictive accuracy of 91.9% (AUROC=0.825, p<.001). The model predicting DD in Parkinson’s Disease patients (n=91) yielded a predictive accuracy of 89.0% (AUROC=0.853, p<.001). Age was a significant predictor of DD across all patients (OR=1.11, p<.05) and BMI was a significant predictor of DD amongst Parkinson’s Disease patients (OR=1.16, p<.05).
Conclusions: It was possible to accurately predict the discharge disposition of DBS patients using routinely collected preoperative clinical variables. The predictive algorithms were applied in the form of a model-driven DSS to assist in improving clinical decision making, healthcare resource planning and patient safety. Expanded multicenter datasets are being compiled to assess more detailed correlations with postoperative risk and costs.
References: Porter, M.E., A strategy for health care reform—toward a value-based system. New England Journal of Medicine, 2009. 361(2): p. 109-112. Boachie-Adjei, O., et al., Surgical Risk Stratification Based on Preoperative Risk Factors in Severe Pediatric Spinal Deformity Surgery. Spine Deformity, 2014. 2(5): p. 340-349.
To cite this abstract in AMA style:
F. Farrokhi. Predicting patient risk and discharge disposition subsequent to deep brain stimulation surgery [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/predicting-patient-risk-and-discharge-disposition-subsequent-to-deep-brain-stimulation-surgery/. Accessed July 9, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/predicting-patient-risk-and-discharge-disposition-subsequent-to-deep-brain-stimulation-surgery/