Category: Epidemiology
Objective: To provide an impression of the Parkinson’s disease (PD) diagnosis and treatment gap across 4 decades in rural Sub Saharan Africa (SSA).
Background: PD is a treatable entity with significant improvement of quality of life by medication and multidisciplinary treatment. The wide diagnosis and treatment gap for PD in Lower (Middle) Income Countries shows that this treatable disorder can remain unidentified and/or untreated during a patient’s lifetime. In a north Tanzanian rural community PD prevalence study from 2006, this gap exceeded 75% [1].
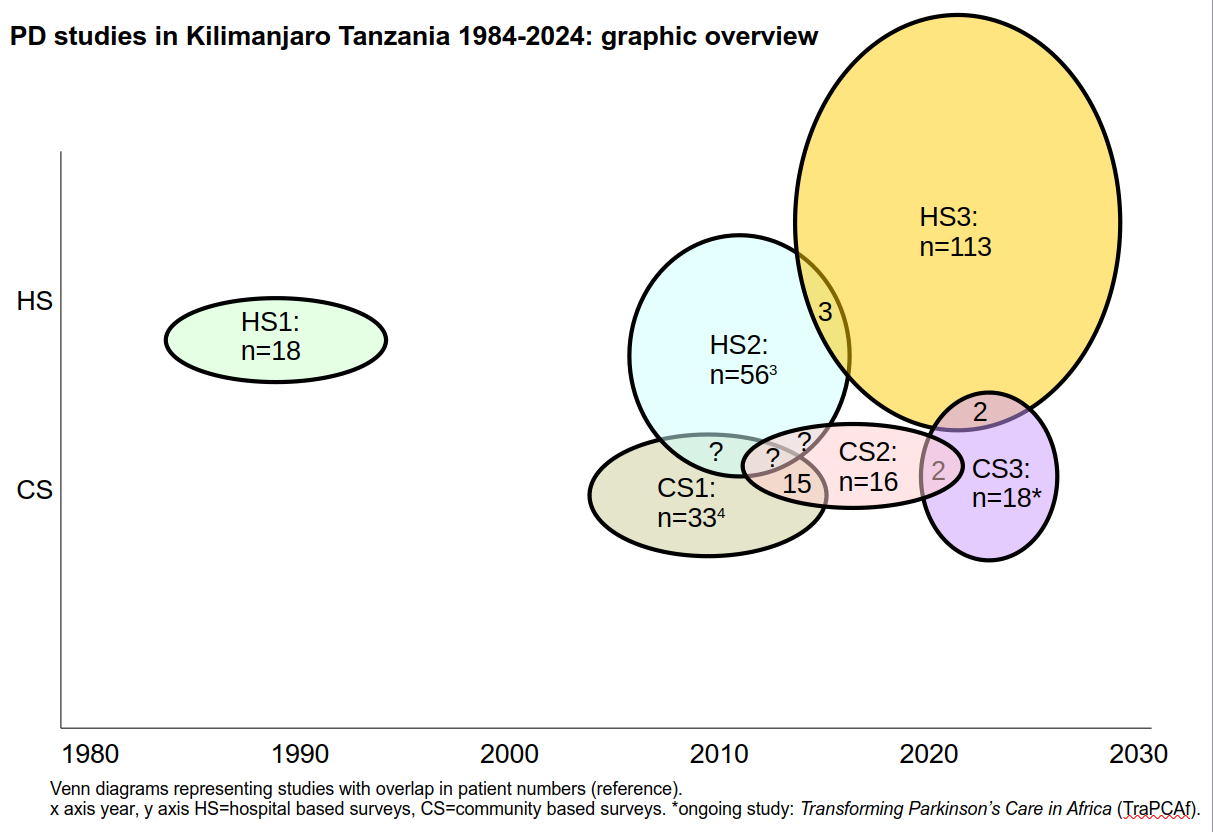
Method: Seventeen years later the survey is being repeated in the framework of the Transforming Parkinson’s Care in Africa (TraPCAf) multinational study across SSA [2] and the present data are an interim analysis of the ongoing survey. Individual patient data were retrieved from 4 subsequent study populations in the same region over 40 years of PD research and graphically represented.
Results: There is an almost total absence of overlap between the populations [figure1] [1,4]. Over fifteen years, overall improvements in healthcare and wealth have occurred with a rise in life expectancy of over 10 years [3] yet provisional data [2] suggests there is a large diagnosis as well as treatment gap of around 70%. As compared with the previous census, the PD mimic vascular parkinsonism has increased representing 40% of parkinsonism patients identified so far [1,5].
Conclusion: Although different study designs cause methodological limitations, persistence of this gap in a small well defined region implies various causes: limited recognition due to PD perceived as a sign of ordinary ageing [6]; disease stigma despite a previous study and community awareness initiatives in the same region; unavailable medication; increased mortality. TraPCAf has initiated further events within Northern Tanzania to raise awareness in both communities and stakeholders within the last few months in an attempt to address this gap, including the first ever PD Patient Support Group in Tanzania. Just as with HIV, optimal utilisation of diagnostic and therapeutic opportunities in a socioculturally stigmatised disorder can still improve over time [1,5]- but may take longer than can presently be analysed. PD is part of a surge in treatable non communicable diseases in SSA, evidence of which is an over representation of vascular parkinsonism attributed to untreated hypertension and or diabetes.
Figure 1
References: [1] Dotchin C, Msuya O, Kissima J, Massawe J, Mhina A, Moshy A, Aris E, Jusabani A, Whiting D, Masuki G, Walker R (2008)The prevalence of Parkinson’s disease in rural Tanzania. Mov Disord 23, 1567-672. doi: 10.1002/mds.21898. PMID: 18581482.
[2] Walker R, Fothergill-Misbah N, Kariuki S, Ojo O, Cilia R, Dekker MCJ, Agabi O, Akpalu A, Amod F, Breckons M, Cham M, Del Din S, Dotchin C, Guggsa S, Kwasa J, Mushi D, Nwaokorie FO, Park T, Rochester L, Rogathi J, Sarfo FS, Shalash A, Ternent L, Urasa S, Okubadejo N. Transforming Parkinson’s Care in Africa (TraPCAf): protocol for a multimethodology National Institute for Health and Care Research Global Health Research Group project. BMC Neurol. 2023 Oct 19;23(1):373. doi: 10.1186/s12883-023-03414-0. PMID: 37858118; PMCID: PMC10585779.
[3] [10] https://www.gapminder.org/ Accessed September 13, 2022.
[4] Howlett WP, Urasa SJ, Maro VP, Walker RW, Kilonzo KG, Howlett PJ, Dekker MCJ (2022) Neurological disorders in Northern Tanzania: A 6-year prospective hospital-based case series. Afri Health Sci 22, 269-84. https://dx.doi.org/10.4314/ahs.v22i1.34
[5] George P, Roushdy T, Fathy M, Hamid E, Ibrahim YA, El-Belkimy M, Abdulghani MO, Shalash A. The clinical and neuroimaging differences between vascular parkinsonism and Parkinson’s disease: a case-control study. BMC Neurol. 2024 Feb 6;24(1):56. doi: 10.1186/s12883-024-03556-9. PMID: 38321372; PMCID: PMC10845551.
[6] Mshana G, Dotchin CL, Walker RW (2011) We call it the shaking illness: perceptions and experiences of Parkinson’s disease in rural northern Tanzania. BMC Publ Health 11, 219. doi: 10.1186/1471-2458-11-219
To cite this abstract in AMA style:
M. Dekker, S. Urasa, W. Howlett, R. Morton, J. Josephat, R. Walker. Rural Tanzania’s Wide “PD Gap” Through the Decades [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/rural-tanzanias-wide-pd-gap-through-the-decades/. Accessed July 3, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/rural-tanzanias-wide-pd-gap-through-the-decades/