Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To understand the impact of the comorbidities; namely Type 2 Diabetes Mellitus (DM) and/or cardiovascular disease (CVD) on the clinical features of Parkinson’s disease (PD).
Background: While aging remains the predominant risk factor for PD, existing evidence favors that DM and CVD play a relatively modest role (1, 2). Elevated risks for all these are believed to be influenced by factors such as hyperglycemia, insulin resistance, low-grade inflammation, increased production of reactive oxygen species, and advanced glycation end products (1). In the case of PD, patients (PwP) cannot afford additional factors contributing to neuronal dysfunction.
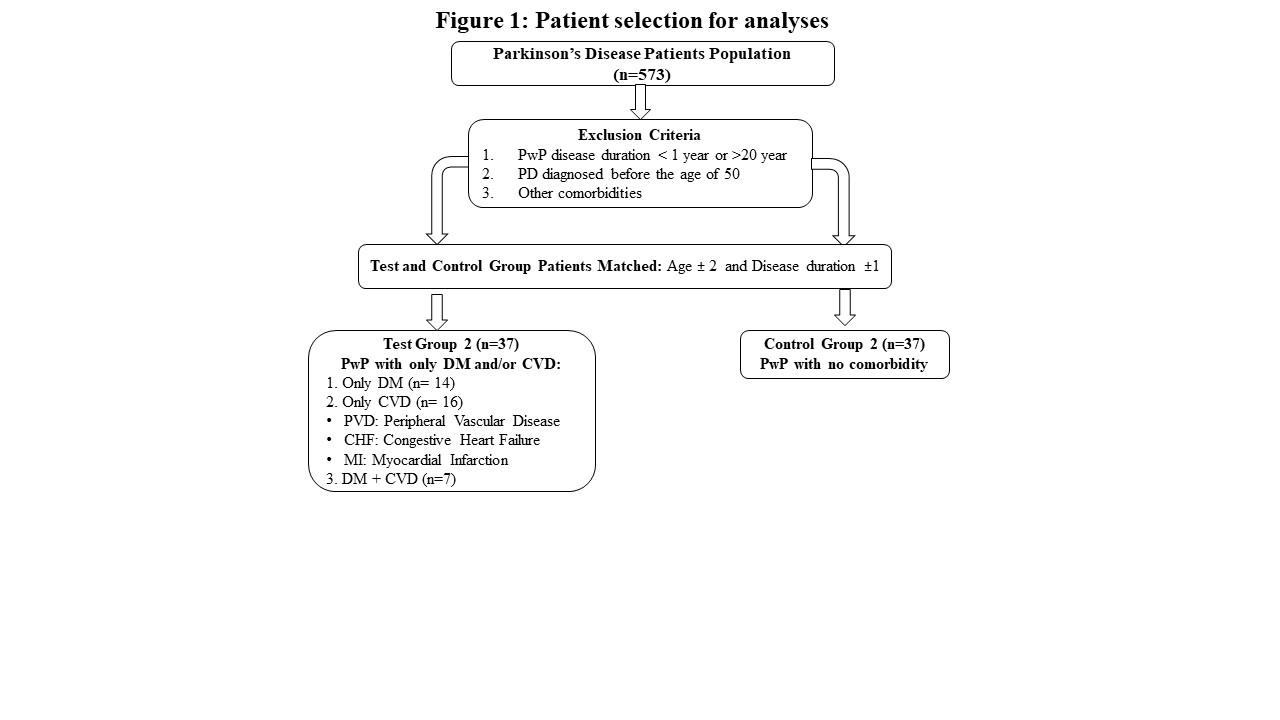
Method: Detailed clinical data from PwP collected between September 2020 and June 2023 were screened. Comorbidities were determined according to the Charlson Comorbidity Index (CCI). PwP were assigned into two groups with only DM and/or CVD (PwP+DM/CVD) and with no comorbidity (PwP-nC). PwP with a disease duration of less than 1 year (for more accurate PD diagnosis), more than 20 years (to avoid accompanying conditions that may confound study results in long-term PD), and PD diagnosed before the age of 50 (3) (to avoid monogenic PD) were excluded. Further, the two groups were matched in terms of age (± 2 years), sex, and disease duration (±1 year). A comparison of the groups regarding a protocol of detailed clinical assessments including motor, and non-motor symptoms, mobility, and quality of life (Figure 1).
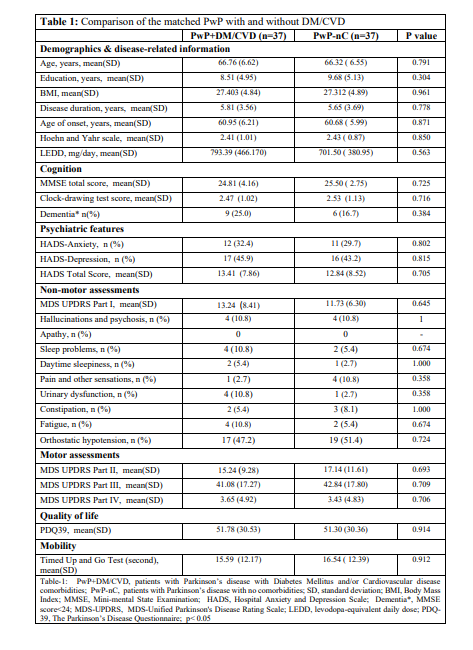
Results: Following the exclusions, matching the two groups yielded 37 PwP+DM/CVD and 37 PwP-nC. None of the compared factors showed significant differences between the groups (Table 1).
Conclusion: In our study, a significant difference was found in none of the analyzed clinical features between the PwP+DM/CVD and PwP-nC groups, questioning the impact of DM and CVD on the course of PD. While the groups were meticulously matched and the clinical evaluations were performed in detail, comorbidities were obtained using self-reported CCI. Additional studies are needed to fully understand the role of low-grade systemic inflammation, insulin resistance, or cardiovascular well-being on synucleinopathies.
Figure 1
Table 1
References: 1. Potashkin J, Huang X, Becker C, Chen H, Foltynie T, Marras C. Understanding the links between cardiovascular disease and Parkinson’s disease. Mov Disord. 2020;35(1):55-74. Epub 20190904. doi: 10.1002/mds.27836. PubMed PMID: 31483535; PubMed Central PMCID: PMC6981000.
2. Athauda D, Evans J, Wernick A, Virdi G, Choi ML, Lawton M, et al. The Impact of Type 2 Diabetes in Parkinson’s Disease. Mov Disord. 2022;37(8):1612-23. Epub 20220614. doi: 10.1002/mds.29122. PubMed PMID: 35699244; PubMed Central PMCID: PMC9543753.
3. Kolicheski A, Turcano P, Tamvaka N, McLean PJ, Springer W, Savica R, et al. Early-Onset Parkinson’s Disease: Creating the Right Environment for a Genetic Disorder. J Parkinsons Dis. 2022;12(8):2353-67. doi: 10.3233/jpd-223380. PubMed PMID: 36502340; PubMed Central PMCID: PMC9837689.
To cite this abstract in AMA style:
T. Abali, SN. Kibrit, Z. özdamar, İ. Köker, AV. Karacan, MK. Yekedüz, R. Yilmaz, FT. Eminoglu, MC. Akbostancı. The effect of Diabetes Mellitus and Cardiovascular disease on Parkinson’s disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/the-effect-of-diabetes-mellitus-and-cardiovascular-disease-on-parkinsons-disease/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-effect-of-diabetes-mellitus-and-cardiovascular-disease-on-parkinsons-disease/